Colon cancer, or colorectal cancer, refers to cancer that develops in polyps in the inner lining of your colon. It may not cause symptoms right away. Common symptoms include belly pain that doesn’t go away or blood on or in your poop. Colon cancer screening tests to find cancer early on and early treatment may cure it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
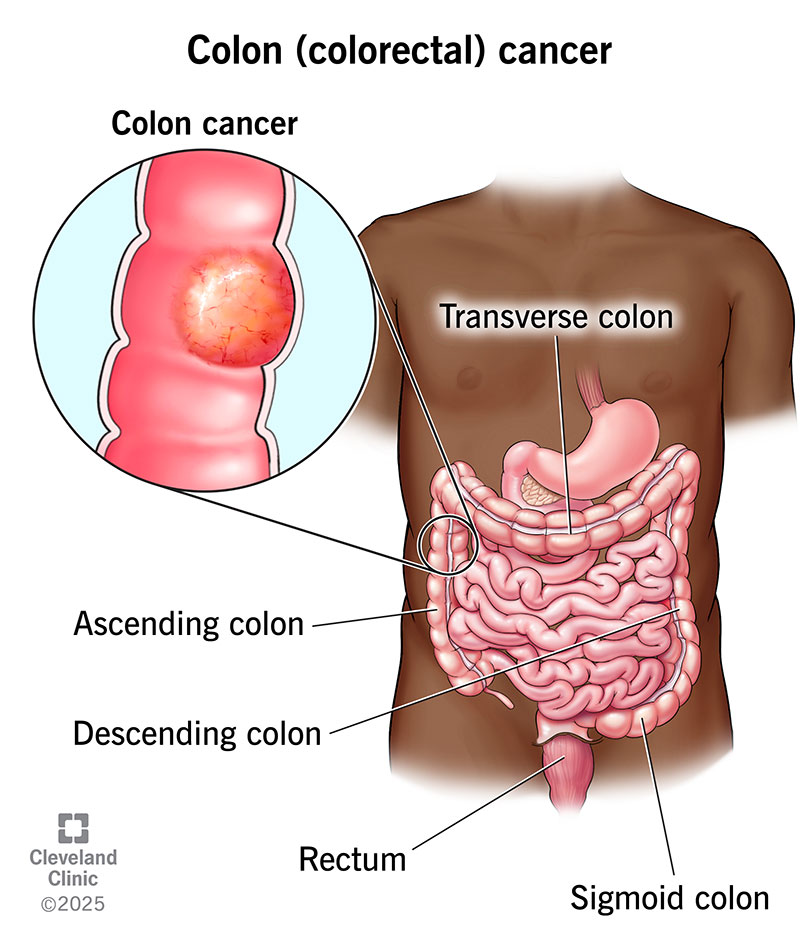
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14501-colorectal-cancer)
Colon (colorectal) cancer is cancer that starts in polyps on the inner lining of your colon and rectum. Colon cancer is a type of cancer that can affect your colon or your rectum in your large intestine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Polyps in your colon can become cancerous. Cancerous polyps may grow from your colon’s inner lining to spread to other areas of your body. Healthcare providers can do tests, like colonoscopies, that can detect colon polyps before they become cancerous. The tests also detect cancerous colon polyps.
Colon cancer is a serious condition. But removing precancerous polyps can stop colon cancer before it starts. An early diagnosis and treatment to remove cancerous polyps may cure the disease.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_9ywas9f1/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn the six most common signs of colon cancer.
Colon cancer develops slowly. It takes about 10 years for a precancerous polyp to turn into a cancerous polyp that may cause symptoms. When symptoms appear, they may include:
Common conditions, like stomach flu or food poisoning, can make your gut hurt and cause constipation and diarrhea. Having them doesn’t mean you have colon cancer. But talk to a healthcare provider if these issues last for more than a few days. And don’t hesitate to talk to a provider if you spot blood in your stool, lose weight without trying or feel tired, no matter how much rest you get.
Advertisement
Colon cancer happens when genetic mutations turn healthy colon cells into cancerous cells. The cancerous cells divide and multiply to make cancerous colon polyps. Over time, cancer grows through the layers of muscle and tissue that make up your colon wall. Eventually, the cancer breaks through your colon wall and begins to spread outside your colon.
Medical researchers aren’t sure what triggers the change in colon polyps. Research shows certain factors increase your risk. Examples of risk factors include:
A healthcare provider will ask about symptoms, like what they feel like and when you first notice them. They may feel your belly for masses or organs that are larger than normal, or do a digital rectal exam.
Tests include:
These tests do more than diagnose colon cancer. Test information will help your cancer care team set a cancer stage. Cancer staging involves factors like where you have a cancerous colon polyp, if cancer is in your lymph nodes or has spread from your colon to other organs.
There are four colon cancer stages.
| Colon cancer stage | Details |
|---|---|
| Stage 0 | This stage refers to abnormal or precancerous cells in colon polyps. |
| Stage I | There’s a cancerous polyp in your colon wall. |
| Stage II | This stage has three substages: Stage IIA: Cancer has spread through most of your colon wall but hasn’t grown into the wall’s outer layer. Stage IIB: Cancer has spread into the outer layer of your colon wall or through the wall. |
| Stage III | Cancer spreads to your colon wall, lymph nodes or the outer layer of your colon. |
| Stage IV | There’s cancer in other, more distant areas of your body. You may have cancer in lymph nodes that are far from your colon, or parts of your body like your liver, lungs or ovaries. |
| Colon cancer stage | |
| Stage 0 | |
| Details | |
| This stage refers to abnormal or precancerous cells in colon polyps. | |
| Stage I | |
| Details | |
| There’s a cancerous polyp in your colon wall. | |
| Stage II | |
| Details | |
| This stage has three substages: Stage IIA: Cancer has spread through most of your colon wall but hasn’t grown into the wall’s outer layer. Stage IIB: Cancer has spread into the outer layer of your colon wall or through the wall. | |
| Stage III | |
| Details | |
| Cancer spreads to your colon wall, lymph nodes or the outer layer of your colon. | |
| Stage IV | |
| Details | |
| There’s cancer in other, more distant areas of your body. You may have cancer in lymph nodes that are far from your colon, or parts of your body like your liver, lungs or ovaries. |
Surgery is the most common treatment for colon cancer that hasn’t spread. The different procedures include:
Advertisement
You may have additional treatment before or after your surgery, including chemotherapy, radiation therapy and targeted therapy.
Talk to a healthcare provider if you have belly pain that doesn’t go away or see blood in the toilet or on toilet paper after you poop. Many things may cause these symptoms, including colon cancer. That’s why your provider may do tests to find out what’s going on in your digestive system.
If tests detect colon cancer, you may want to ask your provider questions, including:
Colon cancer survival rates estimate the percentage of people who are alive five years after diagnosis. The National Cancer Institute (U.S.) tracks colorectal cancer survival rates based on the cancer location at diagnosis:
Advertisement
Cancer survival rate information can be confusing. It’s important to remember that these rates are estimates. They reflect the experiences of many other people who have colon cancer. Your experience may be different. Your cancer care team knows survival rate data may make you anxious or worried about the future. They’ll take time to explain what a survival rate means in your case.
Research shows that in general, having colon cancer can reduce lifespan by about 10 years. How long you’ll live after your treatment depends on factors like your age, the cancer stage at diagnosis, your treatment and your health.
You may not be able to prevent cancer, but you can reduce your risk of developing the condition by:
Advertisement
Colon cancer grows slowly. It may take years before you have symptoms. That’s why tests to screen for colon cancer are so important. The tests often detect colon polyps that could become cancerous or a cancerous polyp that’s spreading in your colon.
You may be anxious or upset if tests show you have colon cancer. Take some time to understand your diagnosis. You may have lots of questions about what to expect. Your cancer care team will be there to answer them, explain recommendations and support you throughout diagnosis and treatment.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Colorectal cancer can turn your world upside down. At Cleveland Clinic, our experts will craft a treatment plan to help you get the best care possible.
