Aortic valve surgery is a lifesaving treatment for aortic valve disease. A surgeon repairs or replaces a damaged valve that connects your heart to your aorta. This improves heart function in people with a narrowed or leaky aortic valve. Surgeons use open-heart or minimally invasive methods. New valves come from animal tissue or human-made materials.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
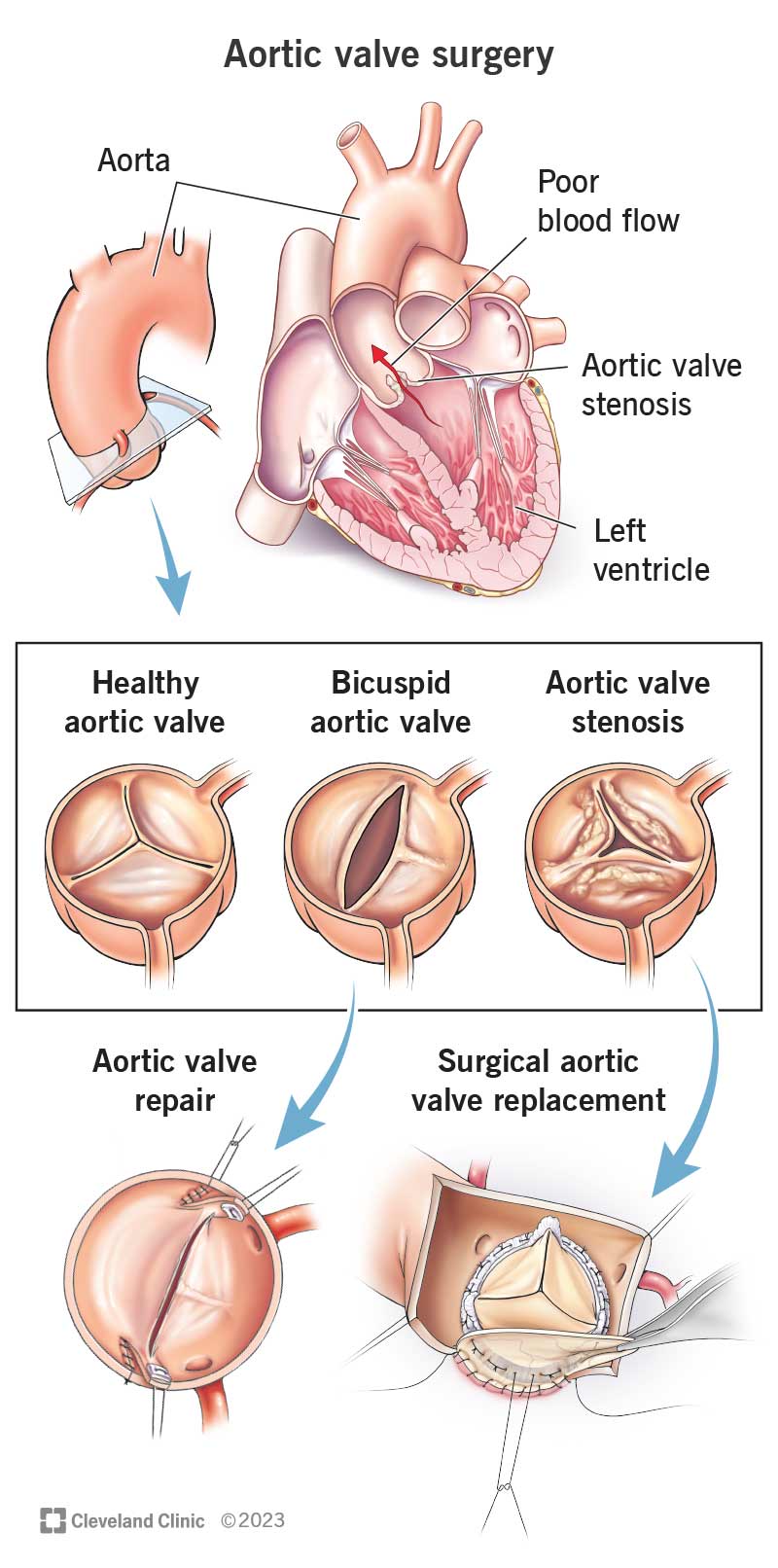
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16745-aortic-valve-surgery)
Aortic valve surgery is a treatment for aortic valve disease. It involves repairing or replacing your aortic valve. This “door” manages blood flow from your heart’s main pumping chamber (left ventricle) into your main artery (aorta). Your aorta sends oxygen-rich blood to your entire body, so it’s important that your aortic valve works well.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Aortic valve disease prevents your aortic valve from functioning as it should. Your valve opening may be too narrow, which limits how much blood can flow through. Or your valve may be leaky, which means some blood flows backward each time your valve closes. Some people are born with congenital heart conditions that may affect valve function.
Cardiac surgeons perform aortic valve surgery to treat:
Although the thought of aortic valve surgery may be overwhelming, an operation can address the valve issue you have. It can also lower your risk of complications of valve disease, like heart failure and cardiac arrest. Thousands of people have had successful aortic valve surgery.
Since aortic valve surgery takes multiple weeks of recovery afterward, it falls into the “serious” category. It also qualifies as “serious” because of the important role your aortic valve plays in getting oxygen-rich blood to your body.
There are two main types of aortic valve surgery:
Advertisement
Many factors determine the type of surgery you need, including:
Your surgeon will talk to you about your options and explain the most appropriate treatment plan for you. If you’re getting a heart valve replacement, you may receive a valve made of animal or human tissue. Another option is a mechanical valve. Each type has its pros and cons, so be sure to discuss these with your surgeon.
In addition to giving you a physical exam, your healthcare provider may order tests before your surgery. Possible tests include:
Your provider will give you instructions that you should follow closely. These instructions will tell you:
Ask your provider if anything is unclear. It’s important to understand exactly what you need to do before your surgery.
To perform aortic valve surgery, your surgeon and care team will:
The exact details of your surgery depend on the surgical approach.
Approaches to aortic valve replacement or repair surgery include:
The most suitable method for you depends on many factors, including:
Advertisement
Your surgeon will talk to you about the approach that’s best for you, and why.
Aortic valve surgery takes at least two hours. The length of time varies by the type of surgery you have.
Here’s what you can expect after your surgery:
Aortic valve surgery is lifesaving. It fixes problems with your heart valve that, over time, could be fatal without treatment. Aortic valve disease is the deadliest form of valve disease. It accounts for more than 60% of all deaths from any type of valve disease.
So, surgery to repair or replace your aortic valve can help you live longer. It can also relieve symptoms so you feel better day to day.
Transcatheter aortic valve replacement (TAVR) has a 92% success rate. For aortic valve repair, multiple studies have reported high survival rates without the need for a second operation for most people.
Advertisement
Like all surgeries, aortic valve surgery has some risks. Possible complications include:
Risks are higher for some people compared to others. Factors that influence your risk for complications include:
Talk to your healthcare provider about your level of risk and how to lower it.
Nonsurgical treatments like medications may help manage your aortic valve disease for a long time. But you may need surgery if you have symptoms, evidence of heart damage or heart failure. That doesn’t mean you need open-heart surgery, though. You may be a candidate for a type of aortic valve replacement your surgeon can do without opening your chest.
Recovery from aortic heart valve surgery generally takes four to eight weeks. It may be shorter if you have minimally invasive surgery.
You can expect to feel tired for a few weeks after your surgery. That’s normal, and it’s important not to push yourself. Still, it’s also important to follow your healthcare provider’s guidance for exercise, including cardiac rehab. A gradual, safe return to movement will support your recovery and long-term health. Your provider will tell you when it’s safe to drive or lift heavy objects.
Advertisement
Remember that each person’s recovery is unique. Try not to compare your recovery or how you’re feeling to others who’ve had heart surgery. If you need more time to feel normal again, that’s OK. Give your body the time it needs to rest and heal.
You can expect to have a follow-up appointment with a healthcare provider during the first week after your surgery. You’ll have another visit about six weeks after surgery. After that, you’ll return as often as your provider recommends.
Some people experience depression after heart surgery. This is common and treatable. Talk to your healthcare provider or a counselor if you have symptoms of depression. These may include feeling very sad or hopeless or losing interest in your usual activities.
You can return to work in about six to 12 weeks. This can vary depending on the type of surgery you have and the type of work you do. If you have a job that’s physically demanding, you’ll need more time to recover.
Call your healthcare provider if you have signs of complications, like:
The thought of someone operating on your heart can make you uneasy. Talk to your healthcare provider about the benefits and risks of aortic valve surgery in your situation. Make sure you understand exactly what’s involved and what your outlook will be after the surgery. You may also want to ask your surgeon about the number of surgeries they’ve performed and their success rate. Having surgery at a high-volume hospital that commonly treats aortic valve disease can help you get the best possible outcome.
As you plan your surgery, talk to your family and friends about it. Offer them chances to help you prepare and recover. Having a support system close by can aid your physical and emotional recovery from this major life event.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have aortic heart valve disease, you want the best care. Cleveland Clinic is number one in the nation for heart health. We’re ready to help you.
