Peripheral neuropathy refers to any condition that affects the nerves outside your brain or spinal cord. This can happen for several reasons, from trauma to infections to inherited conditions. There are also many possible symptoms. Many causes, forms or symptoms of this condition are treatable, but this can vary widely from person to person.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
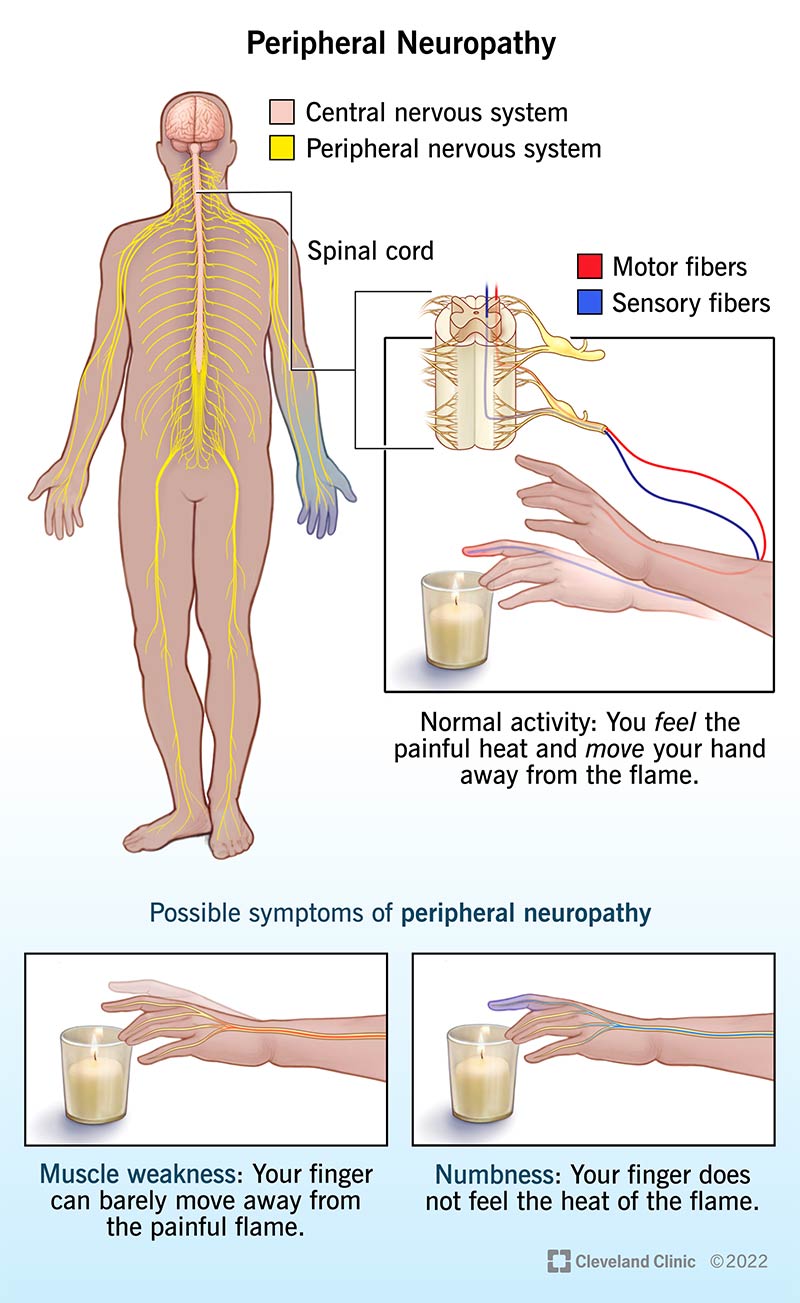
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14737-peripheral-neuropathy.jpg)
Peripheral neuropathy is an umbrella term for nerve diseases that affect a specific subdivision of your nervous system. Many different conditions can cause peripheral neuropathy, which means a wide range of symptoms is also possible. Peripheral neuropathy can also affect different body parts, depending on how and why it happens.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The term “peripheral” is from the Greek word that means “around.” “Peripheral” in this context means outside of or away from the “central” nervous system. The term neuropathy combines two words that trace their origins back to ancient Greek:
Your nervous system has two parts, the central nervous system and the peripheral nervous system. Your brain and spinal cord are the two components that make up your central nervous system. Your peripheral nervous system consists of all the other nerves in your body. It also includes nerves that travel from your spinal cord and brain to supply your face and the rest of your body.
Peripheral neuropathy can refer to any condition affecting your peripheral nerves. Healthcare providers often use the terms “neuropathy” and “polyneuropathy” (meaning “disease of many nerves”) interchangeably with “peripheral neuropathy.” Peripheral nerves are farthest from the central nervous system, and they often show the earliest and most severe effects of these conditions
Peripheral neuropathy can affect anyone, regardless of age, sex, race or ethnicity, personal circumstances, medical history, etc. However, some people are at greater risk for specific types of peripheral neuropathy (see below under Causes and Symptoms for more about this).
Advertisement
Peripheral neuropathy is also very common with some age-related diseases. That means the risk of developing peripheral neuropathy increases as you get older.
Peripheral neuropathy is common, partly because this term refers to so many conditions. About 2.4% of people globally have a form of peripheral neuropathy. Among people 45 and older, that percentage rises to between 5% and 7%.
To understand how peripheral neuropathy affects your body, it helps to know a little about the structure of neurons, a key type of cell that makes up your nerves. Neurons send and relay signals through your nervous system using electrical and chemical signals. Each neuron consists of the following:
Peripheral neuropathy happens in two main ways:
How peripheral neuropathy develops, particularly the timeline of its progress, depends very much on what causes it. Injuries can cause it to develop instantaneously or within minutes or hours. Some toxic and inflammation-based forms of peripheral neuropathy may develop rapidly over days or weeks, while most other conditions take months, years or even decades to develop.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_b7bgpswl/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn more about peripheral neuropathy.
There are many different symptoms of peripheral neuropathy. This condition can affect a single nerve, a connected group of related nerves, or many nerves in multiple places throughout your body. The symptoms also depend on the type of nerve signals affected, and multiple signal types may be involved.
Advertisement
The symptom types (with more about them below) are:
Your peripheral nervous system carries motor signals, which are commands sent from your brain to your muscles. These signals are what make it possible for you to move around. Your muscles need nerve connections to the brain to stay healthy and work properly.
Motor symptoms include:
Your peripheral nerves convert information about the outside world into nerve signals. Those signals then travel to your brain, which processes those signals into what you can sense of the world around you. Peripheral neuropathy can disrupt what your senses pick up from the outside world or the ability of those senses to communicate with your brain.
Advertisement
The sensory symptoms of peripheral neuropathy include:
Advertisement
Your body has several autonomic processes. These are the automatic functions of your body that happen without your thinking or even being aware of them. They include things like sweating, digestion, blood pressure control, etc. Autonomic nerve fibers carry autonomic signals. Disruptions in autonomic signals mean your body’s automatic processes can’t work correctly. Some may work off and on, while others may not work at all.
Autonomic symptoms of peripheral neuropathy can include:
Peripheral neuropathy can happen for many reasons. These include:
Peripheral neuropathy isn’t contagious. While it can happen because of infectious diseases, this condition doesn’t spread from person to person on its own. The only exception is Hansen disease, which can spread from person to person but doesn’t spread easily.
Diagnosing peripheral neuropathy usually involves a combination of methods. These include:
The most common types of tests for peripheral neuropathy (either to confirm the diagnosis or rule out other conditions) include:
The treatment for peripheral neuropathy can vary widely depending on its cause. Other factors can also affect treatment, including your medical history, personal preferences and more. Your healthcare provider is the best person to tell you more about the treatment(s) they recommend and the likely recovery timeline. In general, the following treatment methods are more common for peripheral neuropathy:
The possible side effects and complications of treatments for peripheral neuropathy depend on many factors. These include the specific cause of the neuropathy, other conditions you have, the specific treatments you receive and more. Your healthcare provider is the best person to tell you more about the possible side effects and complications you might experience.
Peripheral neuropathy is a sign of a problem with the nerve signals traveling between parts of your body and your brain. While this can happen for minor reasons that aren’t serious, it can also happen because of severe or dangerous conditions. It’s also sometimes possible to stop or reverse certain types of neuropathies if treatment begins quickly enough. Because of these factors, you shouldn’t try to self-diagnose and self-treat it. A healthcare provider is the best person to guide you in managing this condition.
The effects of peripheral neuropathy depend on the cause, the nerves it affects, your medical history, treatments you receive and more. Your healthcare provider is the best person to tell you more about what you can expect in your case.
Peripheral neuropathy can be a temporary concern, or it can be permanent. How long it lasts depends on what caused it, the extent of the damage — if any — that it caused, the treatments and more.
Peripheral neuropathy is most likely to be permanent with chronic conditions like type 2 diabetes, autoimmune diseases and genetic conditions. However, this can still vary, so it’s best to ask your healthcare provider about what’s most likely in your case.
Peripheral neuropathy is usually not dangerous, but it can have very disruptive effects on your life. These effects are usually not as severe when it only affects one nerve or a limited group of nerves. The more nerves it affects, the greater the potential impact.
The outlook also depends partly on your symptoms. Pain from peripheral neuropathy is usually the most disruptive symptom, but medications or other treatments may help. Autonomic symptoms are among the most serious because they involve your body’s vital functions. When those don’t work correctly, it can have very severe — and sometimes dangerous — effects.
Motor and sensory symptoms can also greatly disrupt your ability to work and go about your daily activities. They can cause problems — sometimes severe — with mobility, balance and coordination. Sensory symptoms are also disruptive, especially when they involve pain or affect your ability to control what you do with the affected body part(s).
Lastly, treatments can make a big difference in outlook. Some treatments can greatly reduce or even stop symptoms, but this varies. Your healthcare provider is the best source of information on the outlook for your case and what you can do to help.
Some of the possible causes of peripheral neuropathy are preventable. You can also lower your chances of developing it by preventing or delaying certain conditions. In general, the best preventive or precautionary steps you can take include:
If you have peripheral neuropathy, it’s important to follow your healthcare provider’s guidance. That includes seeing them as recommended, taking medications or treatments as prescribed and modifying your life to protect yourself and manage your symptoms. The actions you can take also vary widely depending on many factors, and what helps one person may not be as effective for another.
If you have symptoms of peripheral neuropathy, you should see a healthcare provider as soon as possible. In some cases, peripheral neuropathy symptoms start before the condition causes permanent changes or damage, so it may be possible to limit the effects or even reverse them.
If you receive a diagnosis of peripheral neuropathy, you should see your healthcare provider as recommended or if you notice changes in your symptoms. You should also talk to them if you experience side effects from any treatments. Talking to your healthcare provider can be especially helpful when you have symptom changes or side effects that affect your usual routine and activities. Your provider may be able to modify your treatment or find ways to adapt to these changes and limit their effects.
In general, peripheral neuropathy isn’t likely to cause life-threatening complications or symptoms. However, there are a few conditions that fall under peripheral neuropathy that are severe and need immediate medical attention.
There are also conditions that share symptoms with peripheral neuropathy. You should go to the ER if you have symptoms of certain conditions that can be especially dangerous, such as:
You should also go to the ER if you have autonomic symptoms of peripheral neuropathy, such as:
Peripheral neuropathy may be reversible in some cases, but many factors influence whether or not this is possible. Because there are so many factors involved, your healthcare provider should be the one to answer this question for you. The information they provide will be the most accurate and relevant for your specific case and circumstances.
Fatigue is a symptom that can happen with conditions that can cause peripheral neuropathy. It can also happen due to living with severe or long-term pain due to peripheral neuropathy, or because of autonomic problems from peripheral neuropathy. However, it isn’t a direct symptom of peripheral neuropathy itself.
Peripheral neuropathy can be serious, but there are many reasons why it might not be. Whether or not it’s serious depends on many factors, including the symptoms it causes, how severely it affects nerves and more. Your healthcare provider is the best person to tell you about the seriousness of your case and what that means for you.
Peripheral neuropathy isn’t something you can self-diagnose. A qualified and trained healthcare provider can diagnose it, but the diagnosis process almost always involves some form of diagnostic, imaging or laboratory testing. You may suspect you have peripheral neuropathy based on the symptoms you experience, but you should see a healthcare provider to be sure.
There’s no one common treatment for peripheral neuropathy. The treatments depend on what’s causing it and the symptoms you experience. Some causes of peripheral neuropathy are directly treatable. For others, treating and minimizing the symptoms and their effects is the best approach.
Yes, peripheral neuropathy can sometimes go away, but this isn’t universal. Many factors can influence how long peripheral neuropathy lasts. The condition that causes peripheral neuropathy is a major factor in whether or not it will go away, as are the treatments you receive. It’s also important to remember that what works for one person may not work for another, because peripheral neuropathy can happen very differently from person to person.
Peripheral neuropathy is an umbrella term for any condition, disease or disorder that affects your peripheral nerves, which are all the nerves outside of your spinal cord and brain. There are many different ways that peripheral neuropathy can happen, so this condition is common.
For some people, peripheral neuropathy is temporary, treatable or both. For others, it’s permanent and incurable. Thanks to advances in medical science and technology, many symptoms or forms of peripheral neuropathy are now treatable. That offers many people a chance to manage this condition, meaning they can live longer and with fewer restrictions or impacts from the related conditions and symptoms.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Neuropathy, or nerve pain, can make daily life challenging. We can treat the causes of nerve pain and get you back to living life as pain-free as possible.
