Heartburn is a burning sensation that feels like it’s in your heart, but isn’t really. It’s in your esophagus, the swallowing tube that runs alongside your heart. The feeling is caused by acid refluxing up from your stomach. It’s treatable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
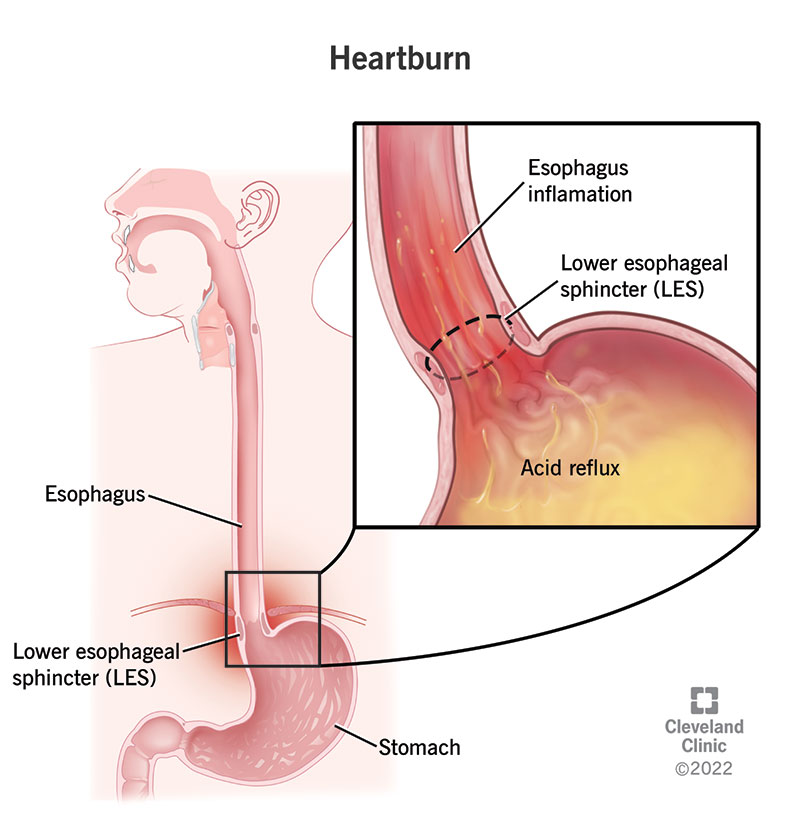
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/9617-heartburn)
Heartburn is a painful, burning feeling in the middle of your chest. It’s not really in your heart, though. It’s caused by stomach acid rising into your esophagus (reflux), which runs through your chest, close to your heart. Heartburn is an occasional symptom for many people, and a chronic condition for others, occurring frequently. When it’s chronic, you might have GERD (gastroesophageal reflux disease).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many people have heartburn occasionally. It can be triggered by an especially rich or acidic meal, or by extra abdominal pressure, such as during pregnancy. Heartburn that occurs regularly is a symptom of chronic acid reflux (GERD), which is also relatively common. Approximately 20% of people in the U.S. have GERD. Risk factors include having obesity (a body mass index or BMI greater than 30) and overweight (a BMI greater than 25), smoking and exposure to second-hand smoke.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_175aljdj/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Heartburn is a painful, burning feeling in the middle of your chest.
Heartburn feels like acid burning in your chest, which is pretty close to what it actually is. Your esophagus, the swallowing tube that begins at your throat, travels down through the middle of your chest to reach your stomach. Heartburn begins in this tube, but the feeling often radiates through your chest and sometimes into your throat. It’s a burning sensation that can be mild to severe.
You may notice heartburn more when:
Heartburn may last anywhere from a few minutes to a few hours. It should go away when the last meal you ate has passed out of your stomach. Once your stomach has emptied its contents, there should be nothing left to come back up (reflux). Depending on the meal, it can take two to five hours for your stomach to finish digesting. Rich and fatty meals take longer to break down in your stomach.
Advertisement
It may be hard to tell the difference between heartburn and other types of chest pain. If you’re unsure about the type of pain you’re feeling, it’s always a good idea to discuss it with a healthcare provider. It may also help to focus on other symptoms that you might have with it. These accompanying symptoms can help you distinguish heartburn from a heart attack or from other esophageal disorders.
If your heartburn is from acid reflux, you may have:
Other atypical symptoms of acid reflux, include:
When related to GERD, heartburn occurs when stomach juices, including acids and enzymes, backwash into your esophagus. Your stomach has a thick mucous lining that protects it from these substances, but your esophagus doesn’t. A valve at the bottom of your esophagus called the lower esophageal sphincter is supposed to keep stomach contents from coming back up. But sometimes it’s weak or doesn’t close all the way.
Different things can cause your lower esophageal sphincter to weaken or relax too much, such as:
Often, more than one of these factors contributes to acid reflux and heartburn.
If heartburn is relatively new to you, and you haven’t recently changed your diet or lifestyle, you may be getting it for other reasons that can develop gradually over time. For example:
Advertisement
Heartburn is usually a disorder of the esophagus with acid reflux as the most likely cause. But there are a few other conditions that can cause the same sensation. For example:
Advertisement
Occasional heartburn is uncomfortable, but it won’t do any real damage. In fact, some amount of acid reflux is normal, and most people don’t even feel it. If you’re feeling it, you may be getting more acid reflux than your esophagus can tolerate. If this happens occasionally, it’s a minor wound that will heal quickly. If it happens regularly though, your esophagus lining may not have enough time to heal in between.
When your esophagus lining is consistently injured, it can lead to long-term complications, like:
Advertisement
Acid reflux that causes heartburn may also indicate other hidden problems in your digestive system. For example, you may have too much acid in your stomach, which can cause complications like gastritis and stomach ulcers. Acid reflux may also aggravate your asthma or other chronic respiratory conditions. If reflux rises into your throat, it can cause swelling and lead to ulcers and growths there.
Heartburn is a feeling that you’ll describe to your healthcare provider. Most providers will recognize heartburn by its description. They may not need to investigate if it’s occasional or mild. But if they suspect you have a chronic condition, they might want to take a look at your esophagus for signs of damage. They may refer you to a gastroenterologist, a specialist in the GI tract, to diagnose you.
Tests to examine your esophagus include:
You can treat occasional heartburn at home with over-the-counter (OTC) medications and lifestyle adjustments. But for frequent heartburn, you might need prescription medications. Medications reduce the acid coming out of your stomach into your esophagus. But they don’t fix the original problem with your lower esophageal sphincter. If medications don’t work, you might need additional treatment.
Medications for heartburn include:
Additional treatments for heartburn might include:
For GERD that doesn’t respond to medication — or as an alternative to long-term medication — your provider might suggest a procedure, such as:
Heartburn is treatable. In the best-case scenario, you may be able to manage it by making some diet and lifestyle adjustments and keeping some antacids handy for occasional use. If you need them, long-term prescription medications are also very effective for acid reflux. Functional disorders can be trickier to manage, but with persistence and a combination of different therapies, they often improve over time.
To help prevent acid reflux:
See a healthcare provider if:
Occasional heartburn is common, and most people can manage it with small adjustments. But if you have it all the time, you may need medical care. Don’t leave chronic heartburn untreated. Pain in your esophagus usually means it’s being injured, and this can do real damage over time. Chronic heartburn may also be a sign of other problems that need treatment. See a healthcare provider about chronic heartburn.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
