Eosinophilic esophagitis is an inflammation of the esophagus caused by an overabundance of certain white blood cells. Food allergies are thought to be one cause of the condition. Among the symptoms of eosinophilic esophagitis are heartburn, chest pain and difficulty swallowing.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
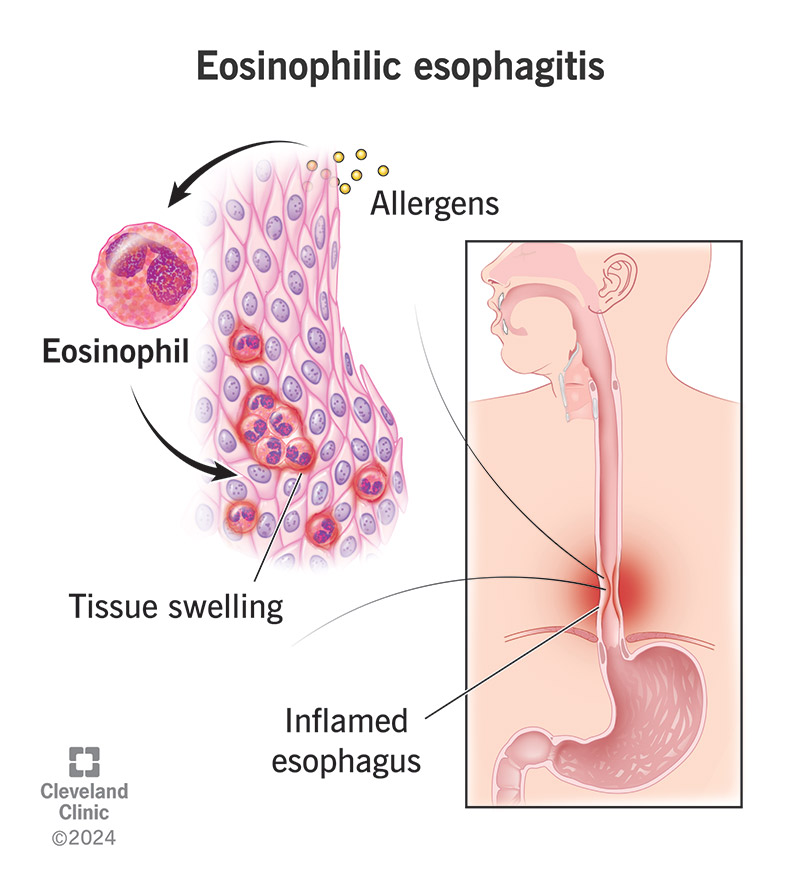
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14321-eosinophilic-esophagitis.jpg)
Eosinophilic (pronounced “e-o-sin-o-FILL-ik”) esophagitis is inflammation in your esophagus, the tube that connects your mouth and stomach.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In this disease, white blood cells (eosinophils) collect in your esophagus and cause inflammation. Without treatment, this inflammation can lead to scar tissue and narrowing in your esophagus, so you have difficulty swallowing. For example, when you take a bite of food, that bite can’t easily move through your esophagus to your stomach. You may feel like something is stuck or moving slowly through your esophagus.
Eosinophilic esophagitis may cause heartburn, chest discomfort and regurgitation (spit up of food). Other less common symptoms are abdominal pain, nausea and vomiting.
It’s a chronic (long-term) disease. There’s no cure for it, but there are treatments that help address the inflammation and manage your symptoms. Most people with eosinophilic esophagitis will need treatment for the rest of their lives.
Eosinophilic esophagitis once was rare, but the number of cases is increasing. It affects about 34 in 100,000 people. Anyone — from babies to adults — can have it.
Your symptoms may be different depending on when you develop the disease:
Advertisement
Symptoms that are less common but that may affect people of any age include:
In some cases, people have symptoms that come and go. A healthcare practitioner may call this a flare-up. But you can also have symptoms all the time.
Eosinophilic esophagitis symptoms may feel like symptoms of more common esophageal disorders. People with this condition may have it for several years before they receive a correct diagnosis.
The disease happens when your immune system reacts to allergens in your esophagus, filling it with inflammatory cells, including eosinophils and cytokines. Allergens can be environmental or food triggers.
The most common food triggers are:
A risk factor is something that increases the chance you’ll have a disease. Many people with eosinophilic esophagitis also have:
Another risk factor is having a family history of eosinophilic esophagitis.
Damage to your esophagus from eosinophilic esophagitis may cause the following complications:
A healthcare provider will do a physical examination and ask about your symptoms. Questions may include:
If a provider thinks you may have eosinophilic esophagitis, they’ll refer you to a gastroenterologist, who can do the following procedures:
Advertisement
Treatment focuses on managing the inflammation in your esophagus. You may receive medication or work with your gastroenterologist to eliminate food groups that trigger inflammation. You and your gastroenterologist will decide what approach works best for you.
Medications to reduce inflammation may include:
In food group elimination, you temporarily stop eating any food from the six common food triggers: dairy, egg, peanuts and tree nuts, seafood and shellfish, soy and wheat. Most people have one to three food triggers. Dairy and wheat are the most common triggers.
Your provider will do follow-up biopsies to see if inflammation in your esophagus is under control. If it is:
Advertisement
Your provider may recommend an elemental diet for short-term use.
You may have food impaction — food that’s stuck in your esophagus — because your esophagus is too narrow for food to pass through. When that happens, your gastroenterologist may use an endoscope to remove the food. And if they feel that it’s safe to do, they can dilate (stretch) your esophagus (endoscopic dilation).
Everyone is different, and each treatment option may not work for everyone. Your gastroenterologist will order upper endoscopies with biopsy to confirm treatment is reducing inflammation. For example, if proton pump inhibitors aren’t effective, your gastroenterologist will recommend other treatment options.
Eosinophilic esophagitis is a chronic and serious illness, but it’s not life-threatening. You’ll probably need treatment for the rest of your life, like taking medication or avoiding specific food triggers.
Advertisement
No, it doesn’t appear to increase the risk you’ll have this kind of cancer.
Living with eosinophilic esophagitis can be challenging. If you’re like most people, your symptoms will go away after treatment for inflammation and reducing scar tissue.
But you may feel anxious or nervous about swallowing food, especially if you experience food impaction (food stuck in your esophagus). You may feel reluctant about taking bigger bites of food when you eat or eating foods, like bread, that you struggled to swallow before your treatment. Some people develop phagophobia (fear of swallowing).
Here are some suggestions that may help you to take care of yourself:
You should follow up at least once a year with your gastroenterologist. You should contact them right away if your symptoms come back or you have new issues with swallowing or food impaction.
Both conditions are types of eosinophilic gastrointestinal disease (EGID). All EGIDs involve high numbers of eosinophils in different parts of your digestive system. Eosinophilic gastritis affects your belly while eosinophilic esophagitis affects your esophagus. Other types are:
A diagnosis of eosinophilic esophagitis may come as a relief, particularly if you’ve had symptoms for years without knowing the cause. But this is a chronic illness, which means you’ll need treatment for the rest of your life. It can be challenging to live with a chronic illness. But it may help to know you aren’t facing the challenge on your own because your healthcare team will be there to help you.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When your child has trouble swallowing food and eating, Cleveland Clinic Children’s can help. We provide eosinophilic esophagitis treatment for kids of all ages.
