Esophagitis is inflammation in your esophagus, the swallowing tube that runs through the middle of your chest. It might feel like chest pain, or it might make swallowing painful or difficult.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
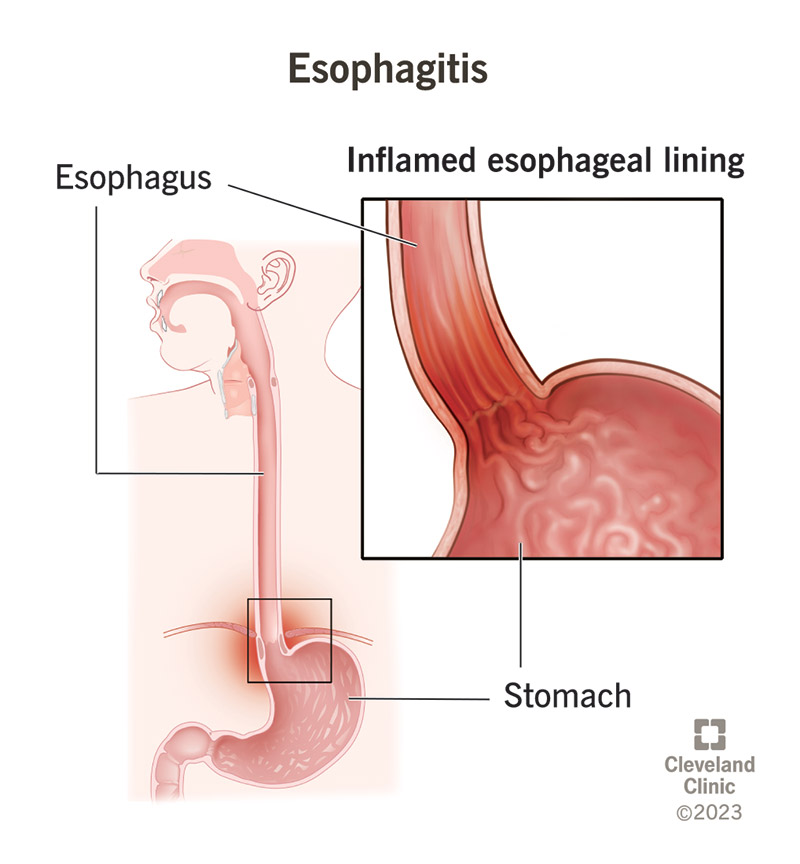
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/10138-esophagitis)
Esophagitis is inflammation in your esophagus, the swallowing tube that runs from your throat down to your stomach. It may feel sore, swollen, raw or burning. Inflammation in your tissues occurs when your immune system has been activated to destroy an infection or allergen or to repair tissue damage. Erosive substances, such as stomach acid and certain medications, can injure your esophagus tissues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chronic acid reflux (GERD) is a common cause of esophagitis. Other types of esophagitis are relatively rare. Esophageal infections are uncommon, except in people who have compromised immune systems.
Esophagitis may feel like:
The pain may be mild to severe and may be constant or come and go.
Depending on the cause and the severity, you might also notice:
Your esophagus tissues might become inflamed if your immune system has been activated to fight an infection, if you’re having an allergic reaction or if something corrosive has injured the tissues.
Causes include:
Different causes make up different subtypes of esophagitis.
The most common type of esophagitis occurs when acids and digestive agents escape your stomach and reflux into your esophagus, irritating and eroding the mucous lining (mucosa). This may happen if you have frequent acid reflux or if you vomit frequently. Causes include:
Advertisement
Also called pill esophagitis, this type occurs when frequently used medications erode the mucous lining of your esophagus. Medicines that may have this effect include:
Infections in your esophagus are uncommon unless you have a weaker immune system and are prone to more frequent and more severe infections in general. When they do occur, infections usually spread to your esophagus from somewhere else. Fungal infections are the most common type, followed by viral infections. Infections that may cause esophagitis include:
Factors that may weaken your immune system, making you susceptible to esophageal infections, include:
Eosinophilic esophagitis is a type of immune hypersensitivity reaction (an overreaction of your immune system). It happens when your immune system sends too many white blood cells (eosinophils) to attack a perceived threat, such as an infection or allergy. The white blood cells accumulate in your esophagus and cause chronic inflammation, even after the perceived threat has passed. This is a rare condition that’s more likely to affect people with multiple allergies.
Besides eosinophilic esophagitis, certain other autoimmune diseases can cause esophagitis as a side effect. These include:
Radiation therapy targeting your esophagus, chest or throat may cause radiation mucositis, inflammation of the mucosa in your esophagus. This is usually a temporary reaction, but rarely, some people develop chronic esophagitis from radiation.
Esophagitis is treatable, but severe esophagitis that goes untreated can lead to serious complications, such as:
Advertisement
A healthcare provider can often diagnose esophagitis based on your symptoms. They might give you a prescription for acid-blocking medications to see if it helps. If it does, they can assume reflux esophagitis. If it doesn’t, they might need to investigate further. They might look inside your esophagus with an upper endoscopy or measure the acid content in your esophagus with an esophageal pH test.
Esophagitis will heal if you can stop what’s irritating your esophagus long enough to let the natural healing process continue. This may require various lifestyle changes or medications, depending on the cause. Medications can also help to protect and promote healing in your esophagus.
Treatment typically includes medication and lifestyle changes.
Medications may include:
Advertisement
Lifestyle recommendations may include:
If you’re confident that the injury that caused it has stopped, your esophagitis may be able to heal on its own after several weeks. But it’s a good idea to get a medical evaluation and opinion. A healthcare provider can confirm the cause of your esophagitis and advise you on treating that particular cause.
It depends on how easily the cause can be addressed. Some persistent cases may take some trial and error with different medications before landing on the right treatment. Once the right treatment begins, healing usually begins immediately. But it may take three to six weeks for esophagitis to heal completely. If the cause is a chronic condition, you may need long-term therapy to manage it.
Advertisement
During recovery, take care to:
Seek healthcare if you have undiagnosed symptoms of esophagitis or if your treatment isn’t working. Sometimes esophagitis has more than one contributing cause that needs to be addressed.
GERD is the most common cause of esophagitis, but not the only cause. And GERD doesn’t always cause esophagitis in everyone. It takes persistent reflux over time to cause an inflammatory response.
Your esophagus runs from your throat to your stomach through the middle of your chest. Unless it’s sore, you’re probably not aware of your esophagus most of the time. If it does become sore, you might not realize it’s your esophagus. It might feel like chest pain or a sore throat. This is your chance to learn about the kinds of things that can harm your esophagus and how to avoid them.
Most people get esophagitis from acid reflux, which affects at least 20% of the population. But overuse of common over-the-counter medications, like NSAIDs, is another common cause. Less common causes include autoimmune disease and infections associated with weakened immunity. Sometimes it’s a combination of these. If you think you have esophagitis, see a healthcare provider for a diagnosis.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Esophageal disorders can cause many symptoms, including heartburn or trouble swallowing. At Cleveland Clinic, we’ll find a treatment that works for you.
