ACC Late Breaking Science: TACTiC Trial
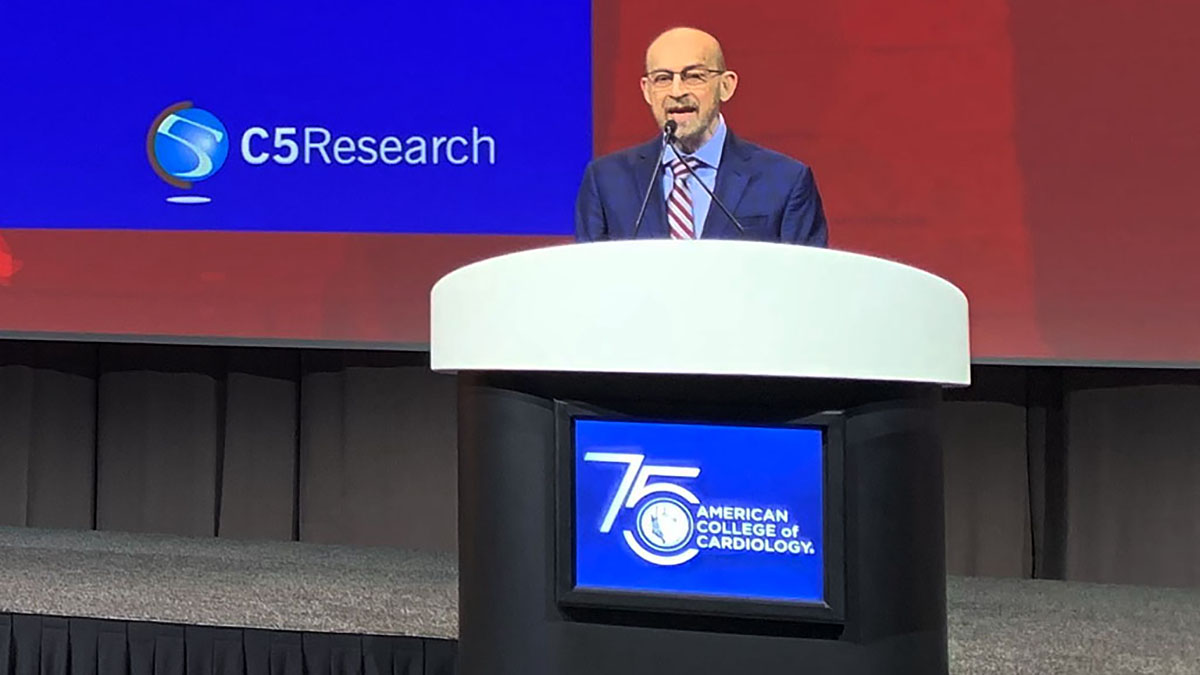
Cleveland Clinic led TACTiC Trial was presented at the American College of Cardiology’s 73rd Annual Scientific Session. Steven Nissen, MD, discusses the results with Katherine Wolski, Lead Biostatistician in the Cleveland Clinic Coordinating Center for Clinical Research (C5Research). C5Research is Cleveland Clinic's Academic Research Organization (ARO) providing academic focus and leadership to the design, planning and management of clinical trials. Dr. Nissen worked with C5Research to investigate if a technology-assisted web application can help consumers appropriately determine if they qualify for a statin drug without a prescription. “Improving cardiovascular health requires increasing access to preventive care for everyone.” - Dr. Nissen.
Subscribe: Apple Podcasts | Buzzsprout | Spotify
ACC Late Breaking Science: TACTiC Trial
Podcast Transcript
Announcer:
Welcome to Cleveland Clinic Cardiac Consult, brought to you by the Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute at Cleveland Clinic.
Steven Nissen, MD:
I'm Dr. Steve Nissen. I am the Chief Academic Officer of the Heart, Vascular & Thoracic Institute, and I'm here with Kathy Wolski, who is the principal biostatistician at C5Research, the research organization for the Heart, Vascular & Thoracic Institute. We're going to talk today about the TACTiC trial. Kathy?
Katherine Wolski:
So Dr. Nissen presented this study at ACC and there will be a simultaneous publication also online. This was essentially a study to look at the role of technology, specifically a web-based application, to assist with consumers being able to purchase a moderate-intensity statin without a prescription.
Steven Nissen, MD:
The really interesting question here is why do this? There have been five prior efforts to develop over-the-counter statins, and they all failed at various stages of development, including a couple of them that went to the FDA for an FDA advisory panel. The question is why they failed. The principal reason they failed is that the wrong people took the drugs. Either the worried well took them who didn't need a statin drug, or people who should not take a statin because of drug interactions or other contraindications took them. And so we really worked on an alternative approach. So maybe, Kathy, you could describe a little bit about how this alternative approach actually works.
Katherine Wolski:
Sure. This was using, again, a technology, a web-based application, where consumers could enter their information, their clinical information, into a web application. So this included medical history laboratory results, especially cholesterol, blood pressure, and then they would enter their information and the app would actually tell them whether they were appropriate to be able to use this five-milligram dose of rosuvastatin. So I think that that is something that is unique that hasn't been done before because it allows us to make sure that we are targeting the right population.
Steven Nissen, MD:
What's interesting about this is behind the scenes, the application is actually calculating their 10-year risk of atherosclerotic cardiovascular disease according to the guidelines. So think of this as a web application that has the guidelines behind that application. What does that do? Well, it ensures that people whose risk is too low will not get an okay to use. People who should not take a statin for a variety of reasons would be excluded.
And it really is an important innovation that makes possible, I think for the first time, a non-prescription access to statins in a way that didn't work for previous efforts. So maybe we can talk about the TACTiC trial. Kathy, you and I were both involved along the way. This was a very difficult study to do. What was done is advertisements were put out, various media asking people if they wanted to consider using cholesterol lowering medication. And then people who responded to those ads were directed to the web app and given the opportunity to enter their data to see if they were in fact able to qualify. Interestingly enough, not surprisingly, a lot of the people were relatively well-educated, and that's not a surprise, although we did include in the trial about 5% of the patients who had low literacy. And it was important to include low literacy participants because anybody can use this application if it's approved. Now, it was in English, and that's a real limitation. If you were non-English speaking, you couldn't really do this. And it required internet access. Almost everybody now has internet access. I'm not sure I know anybody that doesn't have a cell phone or some way to get to the internet, so I don't know that that was a very big limitation. Perhaps we can talk about what the folks look like. Do you have the baseline characteristics?
Katherine Wolski:
Right, yeah. These were consumers who were between the ages of 25 and 75. The average age was about 63. They were mostly white, almost 80% were white, and they came in with a mean LDL at 140. The risk score, the 10-year risk score, was about 10%.
Steven Nissen, MD:
Which is pretty high. I mean, it's certainly right up in the range where a statin would be reasonable. Now, the trial had three primary endpoints. Perhaps you could describe what they were.
Katherine Wolski:
Yeah, sure. The first part of this study really was a self-selection study. Again, we wanted to make sure that we had the appropriate patients. We want to make sure the risk wasn't too low and certainly not too high. The first primary endpoint for this was the concordance between when the patient fills out the web app and when a physician fills out the web app.
Now, the physician doesn't know what the score for the patient was. So the idea was to look at that concordance and make sure that the physician agreed with the patient. So if the patient gets an okay to use, did the physician agree with that based on what he or she knows?
Steven Nissen, MD:
Just one quick note is it could be a non-physician clinician, like a nurse practitioner.
Katherine Wolski:
Yes. Right.
Steven Nissen, MD:
So some healthcare person that had prescribing authority.
Katherine Wolski:
Right, exactly. So then what would happen is if they were okay to use, they could go on to the actual use portion of the study. So there, they go ahead and they order their medication online. This is what's unique about this. We're not talking about taking a set over the counter where you go and you purchase it.
Steven Nissen, MD:
This is an actual use study, meaning it mimics what would happen if it were approved. And so there was a nominal charge to actually receive the medication. We thought that was important to include.
Katherine Wolski:
Right. So then they would enter the actual use phase. They would get their medications. They would have this discussion with a clinician where they would each fill out the web application separately, and then they would be followed for six months. So they're treating for six months. When they needed to reorder, because they were only given a supply of either 45 days or 60 days, so at the time that they need to reorder, they again fill out this tool to make sure they have no conditions that developed that could be contraindicated.
That if they were okay to use, they would get another supply of medication. And at the end of the six-month period, they would again come for a virtual visit. This was all done virtually. They would have another discussion with the clinician. They would again fill out the web app tool. The clinician would fill out the web app tool again. Very separately. And then those results again were looked for concordance. So we wanted to see, one, how many people stayed with us for the six month period. We wanted to see at the end of the day, were they able to get the same results.
Steven Nissen, MD:
So did they have a concordant outcome with the clinician at the end of that six month treatment period?
Katherine Wolski:
Yes.
Steven Nissen, MD:
And then there was a third primary endpoint.
Katherine Wolski:
And of course, the third primary endpoint was the reduction in LDL cholesterol.
Stevenn Nissen, MD:
Now, just for reference's sake, in the prior efforts, less than 50% of people actually correctly used the drug, and we wanted to do better. And the question is, did we? So what was the concordance for the initial self-selection?
Katherine Wolski:
We did really well with that. It was 90%.
Steven Nissen, MD:
Yes. Almost 91%.
Katherine Wolski:
Yeah, almost 91.
Steven Nissen, MD:
90.7%.
Katherine Wolski:
So very, very high.
Steven Nissen, MD:
Very high. We had pre-specified that the lower bound of the confidence interval had to be greater than 85%, and it was. Perhaps even more surprisingly at the end, what was the concordance rate?
Katherine Wolski:
It was over 98%.
Steven Nissen, MD:
It was 98%, and well above that 85% threshold for the lower 95% confidence interval. And then for the third co-primary endpoint, LDL reduction, the hope was that we would get a clinically meaningful LDL reduction. Now, historically, the Food and Drug Administration has required for any drug to be approved for LDL lowering to achieve at least 15% LDL reduction. And in our TACTiC trial, what was the reduction?
Katherine Wolski:
It was over 35%.
Steven Nissen, MD:
Yes. It was really high. And by pill count, the adherence to treatment was about 95%.
Katherine Wolski:
95%.
Stevenn Nissen, MD:
95%.
Katherine Wolski:
Pretty amazing.
Steven Nissen, MD:
Which means that when you ask people to fill out a web app, when they actually purchase a drug online, get the drug shipped to their home, they take it. And we needed to know that they would take the drug and if they would get a really excellent reduction in LDL cholesterol, and they did. Now, there are a couple of things that we didn't talk about that we probably should, which is why do this?
We know that less than half of the consumers who are out there who would qualify for a statin drug, who have not yet had a cardiac event, so this is primary prevention, less than half are actually taking a medication. There's this enormous gap, treatment gap between who should get a statin drug and who's actually getting it. And our hope here was that by providing this non-prescription access, we could close that gap. We could get clinically meaningful reductions in LDL cholesterol for people that maybe aren't getting a medication now. Remember that all these people were not on a statin and they were eligible. There were 1,200 people in this study, but there are millions of people out there that should be on a statin that are not. And so our hope was that by doing this, we could substantially improve the access to statins by a large population of people.
And the question is, who are these people? Well, some of them are people that just don't like to see physicians. Some of them can be people who live in rural areas where in order to see a prescriber, you need to get in the car and travel 20, 30, 40 miles. There are lots of reasons why people don't take statins. We think this could play a really important role in educating consumers about the potential qualification for statins and getting them to the right people.
Now, of course, the FDA has to approve, and the next step is for this trial to be reviewed by the Food and Drug Administration, and we shall see whether or not...
Katherine Wolski:
Do you have a prediction?
Steven Nissen, MD:
I think we worked with the FDA in developing this trial. They set the lower bounds of what they consider to be acceptable. We hit all three endpoints easily in the trial. So I think that with a 1,200 patient study done carefully in collaboration with an academic research organization, our team here at C5Research, that we've achieved the standard. And I think there's a very, very good chance this would become the first time in history that statins would be available to patients without a prescription, and I'm very optimistic that it will help public health.
Announcer:
Thank you for listening. We hope you enjoyed the podcast. We welcome your comments and feedback. Please contact us at heart@ccf.org. Like what you heard? Subscribe wherever you get your podcasts or listen at clevelandclinic.org/cardiacconsultpodcast.

Cardiac Consult
A Cleveland Clinic podcast exploring heart, vascular and thoracic topics of interest to healthcare providers: medical and surgical treatments, diagnostic testing, medical conditions, and research, technology and practice issues.



