Aortic root replacement surgery removes an aneurysm in the part of your aorta closest to your heart and replaces it with a graft. It can save your life by preventing aneurysm dissection or rupture. You’ll either keep your aortic valve (valve-sparing aortic root replacement) or receive a new valve (Bentall procedure).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
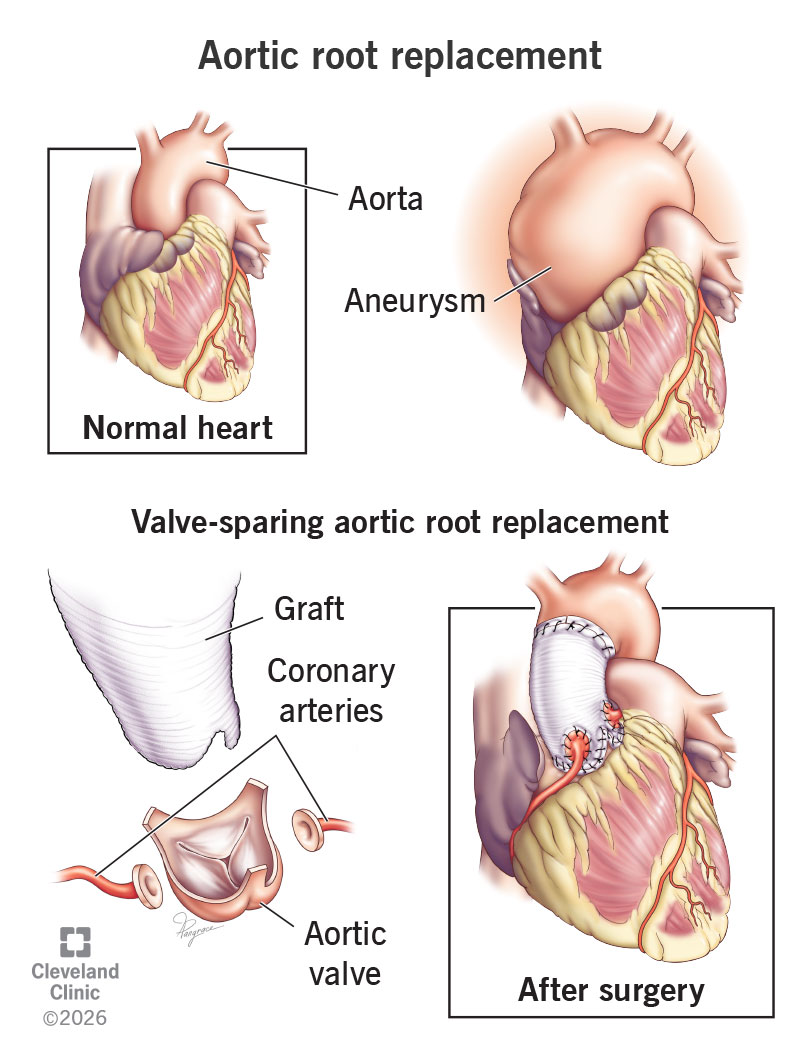
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22821-aortic-root-replacement)
Aortic root replacement is surgery to fix an aneurysm in your largest artery, called your aorta. Specifically, it treats aneurysms in your aortic root. This is the part of your aorta that attaches to your heart. If an aneurysm grows too big or its walls get too weak, it can rupture (break open) or dissect (tear). These are life-threatening complications that surgery can prevent.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
People who have an aneurysm at risk of rupture or dissection may need an aortic root replacement. Sometimes, aging and changes to your aorta over time cause an aortic root aneurysm. Genetic disorders like Marfan syndrome and Loeys-Dietz syndrome can cause potentially fatal aortic aneurysms in younger people.
Your healthcare provider may recommend aortic root replacement if the aneurysm reaches a certain size, typically anywhere from 4 centimeters to 5.5 centimeters. You might need surgery at the lower end of this range if:
The timing of your surgery also depends on other things — like your age, overall health and risk of surgery complications. Factors like unmanaged high blood pressure and smoking can make an aneurysm grow faster. Talk with your provider about your personal risks and how to choose the safest time for your surgery.
There are two main types of aortic root replacement surgery:
Advertisement
Your surgeon will determine the best strategy for you based on many factors, such as the anatomy and function of your aortic valve, your age and overall health status.
Surgeons use a variety of techniques for valve-sparing surgery. Here are two common ones you might hear about:
Preparation is key to a successful surgery, and it starts well before your surgery day. Your healthcare provider will give you a physical exam. They may run tests like:
You’ll also talk with your provider about:
Your provider will give you detailed instructions for your surgery day, including when to stop eating/drinking and any medicines you should take.
To perform an aortic root replacement, your surgeon will:
Advertisement
The Bentall procedure takes about four to five hours. Valve-sparing aortic root replacement is about four to six hours.
A major benefit of aortic root replacement is that it can prevent a life-threatening aneurysm rupture or dissection. Plus, both types of surgery (Bentall and valve-sparing) are successful for most people.
Which type has more benefits for you depends on how well your valve is working and any underlying conditions you have. For example, some research shows people with Marfan syndrome have better outcomes with valve-sparing surgery than with the Bentall procedure.
But like any major surgery, aortic root replacement comes with some risks. These include:
Any open surgery is riskier if you have other serious health problems, including:
Risks vary by person and increase with age. Talk with your provider about your risks and how to manage them.
After your surgery, you’ll spend several days in the intensive care unit (ICU). You’ll then move to a regular hospital room. Most people need to stay in the hospital for about one week total.
Advertisement
While you’re in the hospital, you’ll receive:
Follow your provider’s guidance and take things slow. This healing time helps you get back to normal. You won’t be able to drive until your provider gives you the OK. So, be sure to have someone ready to drive you home.
Full recovery from aortic root replacement surgery takes at least six to 12 weeks. For some people, it can take two to three months. This includes your time in the hospital, at home and in cardiac rehab.
Medicare and most insurance companies cover up to 12 weeks of cardiac rehab. It’s worth your time to use this service. Rehab improves your strength and quality of life after heart surgery. You’ll also be able to meet people who are going through the same thing.
Your surgeon will tell you when it’s safe to return to your usual activities. In general, you shouldn’t drive or lift heavy objects for six weeks. You may be able to return to work after six to eight weeks, but only if your job isn’t physically demanding.
Advertisement
Aortic root replacement is a durable and long-term solution for aortic root aneurysms. How long the valve lasts depends on the type of valve you receive. Mechanical valves last for the rest of your life, but you need to take blood thinners. Tissue valves last at least 10 to 15 years in most people but then may need to be replaced.
If you have valve-sparing aortic root replacement, your natural aortic valve may last for life. But you may need another surgery at some point to get a new valve. It depends on your anatomy and other medical conditions.
Pay attention to your body and how you feel as you recover. Call your provider right away if any of these problems come up:
Incision issues, like:
Signs of a surgery complication, like:
If you have an untreated aortic aneurysm, you’re at risk of rupture or dissection. Call 911 or your local emergency number if you have:
Aortic root replacement is a lifesaving surgery. It protects you from a fatal aneurysm rupture or dissection. Some people need it in their 20s or 30s, while others need it further down the road.
No matter the timing, heart surgery can feel scary and overwhelming. Just remember that this surgery might be your “first,” but surgeons are trained to do them all the time. A successful operation is their top priority. And they’ll do whatever they can to help you feel comfortable from prep through recovery.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you come to Cleveland Clinic for aortic disease treatment, you’ll get industry-leading care and support from our heart and vascular specialists.
