Paraplegia is the symptom of paralysis that mainly affects your legs (though it can sometimes affect your lower body and some of your arm abilities, too). This usually happens because of injuries to your nervous system, especially your spinal cord, but it can also happen with various medical conditions and diseases.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
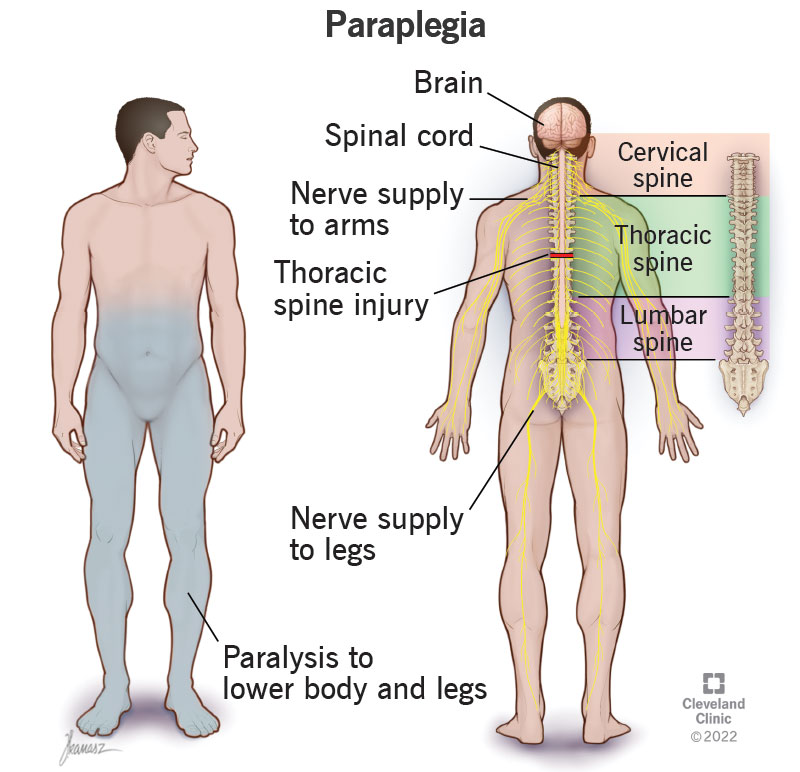
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23984-paraplegia)
Paraplegia is a specific pattern of paralysis (which is when you can’t deliberately control or move your muscles) that affects your legs. This happens because of a problem with your nervous system. Depending on how it happens, this paralysis may have different effects on some body systems or processes. Paraplegia is usually a symptom, but there are rare instances where it’s a specific condition on its own.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are also two main ways that paraplegia can happen, complete and incomplete:
There are also two main ways that paralyzed muscles act in paraplegia:
People with paraplegia have different symptoms depending on how high or low the injury is in their spine. Paraplegia generally affects your legs, but may also affect your abdominal muscles, making it difficult to cough. It can also affect your chest muscles, making it difficult to take deep breaths.
Your spine has multiple sections. Each section has several vertebrae (singular is vertebra). Your vertebrae are interlocking bone segments that make up your backbone and protect your spinal cord.
Advertisement
Paraplegia can happen with injuries in any of the following sections:
Healthcare providers use a letter-number combination to talk about sections of the spine and related spinal nerves. For example, T1 is the spinal nerve that runs between the first and second thoracic vertebra.
The effects of paraplegia generally are as follows:
Paraplegia can happen with problems of your peripheral nerves, which are the nerves that extend outward from your spinal cord. These usually happen because of diseases and conditions that affect multiple nerves at the same time (polyneuropathies), like Guillain-Barré syndrome or diabetes-related nerve damage (neuropathy).
The most common cause of paraplegia is injury to your spinal cord. Those injuries can happen in many different ways. The most common reasons are:
Other common causes of paraplegia include:
Advertisement
The treatments for paraplegia depend on what caused the issue and where it is in your spinal cord. The injuries and conditions that can cause paraplegia can vary widely, and the potential to recover from them can also vary. Because of that, a healthcare provider is the best person to explain the situation. They’ll offer you guidance for your specific situation, including the possible treatments and the side effects or complications that can happen with those treatments.
Paraplegia is a key symptom of a spinal cord injury or a condition that affects your nervous system. These injuries and conditions are almost always medical emergencies. The only exceptions to this are when a healthcare provider diagnoses you with a medical condition that can lead to paraplegia. In those cases, a healthcare provider will provide guidance on what to do if and when paraplegia develops.
IMPORTANT: If you’re with someone who has an injury that could affect their spine, it’s very important that you call 911 (or your local emergency services number immediately) and avoid doing anything that could make the injury worse.
Moving someone with a possible spinal cord injury in the wrong way can cause permanent damage. Because of this, only trained professionals should move someone with a suspected spinal cord injury. The ONLY exception to this is if the person is in immediate danger if you don’t move them (such as from a motor vehicle crash where the vehicle the person is in may catch fire).
Advertisement
Paraplegia is sometimes preventable, but it also happens unpredictably, and in ways you can’t prevent. The best things you can do to prevent paraplegia or reduce your risk of developing it are:
Advertisement
A healthcare provider should ALWAYS examine and treat paraplegia.
Paraplegia is paralysis that affects your legs. Tetraplegia — also known as quadriplegia — is paralysis that affects your arms and legs.
Paraplegia and hemiplegia have a few similarities, but they usually happen in very different ways and for different reasons.
This condition refers to a group of disorders inherited from one or both parents. These disorders disrupt your nervous system, causing paralysis in your legs. The paralysis involves constant muscle movements that a person can’t control (which is why the word “spastic” is part of the name). This condition can happen on its own, or it can happen along with other medical conditions. It’s also progressive, meaning it gets worse over time.
Paraplegia is paralysis that affects your legs, but not your arms. This symptom is most likely to happen with injuries, but can also happen because of diseases or medical conditions. Paraplegia that happens with injuries is a medical emergency and needs immediate medical care. Preventing further injury is critical to reducing the risk of permanent paralysis. While paraplegia can be frightening, there are also many options to help people recover from or adapt to it. Even when paraplegia happens because of permanent damage, it’s possible to adapt and find ways to live independently and have a fulfilling and enjoyable life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Get the care you need today! At Cleveland Clinic, we offer specialty care that’s focused on you.
