Myelomeningocele is a type of spina bifida — a birth defect in which a fetus’s spine and spinal canal don’t close before birth. Healthcare providers can usually diagnose myelomeningocele during pregnancy and perform surgery during pregnancy or after birth to repair the opening in your baby’s spine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
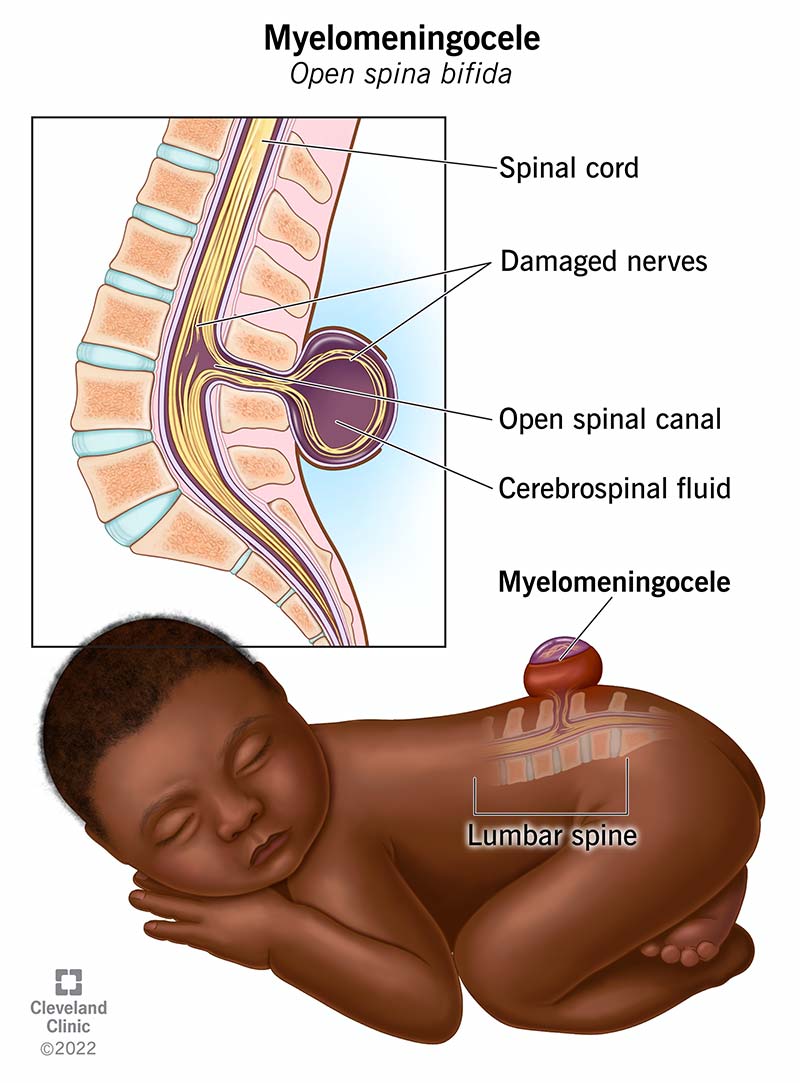
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22813-myelomeningocele)
Myelomeningocele (also known as open spina bifida) is a congenital condition (birth defect) in which your child’s backbone (spine) and spinal canal don’t close before birth. It’s a type of neural tube defect (NTD). Myelomeningocele is pronounced MY-eh-lo-men-IN-go-seal.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Myelomeningocele develops in a fetus during the first four weeks of pregnancy. Myelomeningocele is characterized by incomplete neural tube closure and a fluid-filled sac that protrudes from your baby’s back. The sac contains:
Myelomeningocele can happen anywhere along your baby’s spinal cord. It most commonly occurs in their low back (lumbar and sacral areas).
The part of the spinal cord and the nerves in the sac are damaged, which usually results in weakness and/or loss of sensation to the part of the body below where the sac is located. In some cases, the sac opens up. This can happen due to normal movements of your baby, either before or during birth.
Myelomeningocele is the most serious type of spina bifida and causes moderate to severe disabilities, such as muscle weakness, loss of bladder or bowel control, and/or paralysis. Babies with myelomeningoceles lower in their spine typically have less severe symptoms than babies with myelomeningoceles higher in their spine.
Neural tube defects (NTDs) are birth defects (congenital conditions) of the brain, spine or spinal cord. They happen within the first month of pregnancy — often before you even know you’re pregnant. The two most common neural tube defects are spina bifida and anencephaly.
Advertisement
Normally, during the first month of pregnancy, the two sides of the fetus's spine (backbone) join together to cover and protect the spinal cord, spinal nerves and meninges (the tissues covering the spinal cord). The fetus's developing brain and spine at this point are called the neural tube.
If there’s an issue with the formation of the neural tube, it’s considered a neural tube defect.
Spina bifida refers to any congenital condition (birth defect) in which the neural tube in the area of the spine doesn’t close completely.
Spina bifida can happen anywhere along your child’s spine if the neural tube doesn’t close all the way in utero (in your uterus). When this happens, their backbone, which protects their spinal cord, doesn’t form and close as it should. This often results in damage to your child’s spinal cord and nerves.
Myelomeningocele is a type of spina bifida — the most severe type. It results in a fluid-filled sac that protrudes from your baby’s back that contains part of their spinal cord and nerves. Other types of spina bifida include meningocele and spina bifida occulta.
Myelomeningocele and meningocele are both types of spina bifida. Meningocele happens when a sac of fluid comes through an opening in your baby’s back, but their spinal cord isn’t in the sac. There’s usually little or no nerve damage.
In myelomeningocele, part of their spinal cord and nerves are in the sac and are damaged.
Myelomeningocele can affect any fetus. While scientists are unsure of the exact cause, they’ve identified certain genetic, environmental and nutritional factors that can increase your baby’s risk of developing myelomeningocele.
Myelomeningocele is the most common central nervous system congenital condition, occurring in approximately 1,645 births every year in the United States.
A baby with myelomeningocele will have a fluid-filled sac on their mid- to low-back along their spine. Healthcare providers can usually detect myelomeningocele during pregnancy with an ultrasound.
Other congenital conditions may also be present in an infant with myelomeningocele. Eight out of 10 infants with myelomeningocele have hydrocephalus (fluid buildup in their brain).
Other issues with the spinal cord or musculoskeletal system that are associated with myelomeningocele include:
Healthcare providers and scientists don’t yet know the cause of myelomeningocele, but they believe it’s a complex combination of genetic, nutritional and environmental factors.
Advertisement
In particular, low levels of folic acid in a person’s body before and during early pregnancy appear to play a part in this type of congenital condition. Folic acid (or folate) is important for the fetal development of the brain and spinal cord.
Healthcare providers can usually (but not always) detect and diagnose myelomeningocele in fetuses during pregnancy using the following tests:
Advertisement
Healthcare providers also use imaging tests, such as an MRI (magnetic resonance imaging) or CT (computed tomography) scan, to diagnose myelomeningocele after birth if it wasn’t diagnosed during pregnancy.
Treatment for myelomeningocele typically involves surgery to repair the opening in your baby’s spine.
Healthcare providers can perform surgery before birth (fetal surgery) or shortly after birth (postnatal surgery).
Babies with myelomeningocele often have hydrocephalus (fluid buildup in their brain). Your baby may need a ventriculoperitoneal (VP) shunt placed to help drain the extra fluid from their brain.
Most children will need lifelong treatment for managing issues that result from damage to their spinal cord and spinal nerves. Common treatments include antibiotics to treat or prevent infections such as meningitis or urinary tract infections (UTIs) and physical therapy.
Surgery before birth (fetal surgery) is an option depending on the severity of the myelomeningocele and the health of the person who is pregnant. This type of surgery is becoming increasingly common.
While this surgery may prevent symptoms from getting worse, it can’t correct any damage to the spinal cord or nerves that are already present.
Advertisement
Complications associated with prenatal surgery include increased risk of preterm (early) delivery and uterine dehiscence, a thinning or tearing at the incision in the uterus, at the time of delivery.
If your baby didn’t have fetal surgery to repair the open area of their spine, they’ll need to have postnatal (after birth) surgery as soon as possible to reduce infection risk — ideally within the first 48 hours after birth.
Most children with myelomeningocele benefit from a multidisciplinary team approach for coordinating their care and management. Specialists who may be involved in the care of your child include:
No two people with myelomeningocele are affected in the same way, and the prognosis (outlook) for myelomeningocele depends on several factors, including:
People with spina bifida have a mortality (death) rate of about 1% per year from 5 to 30 years of age. The higher the lesion is on their spine, the greater the risk of complications and mortality.
The side effects and complications of myelomeningocele can greatly impact quality of life. People with myelomeningocele are more likely to develop depression, anxiety and risk-taking behaviors.
Complications associated with myelomeningocele include:
Unfortunately, birth defects like myelomeningocele can’t be prevented — the risk can only be reduced. Most cases of myelomeningocele occur sporadically (randomly), but scientists have identified several risk factors that are linked to the condition, including:
It’s important to remember that having a baby with myelomeningocele isn’t your fault. Every person of childbearing age is at risk of having a pregnancy affected by a birth defect.
It’s important to remember that no two people with myelomeningocele are affected in the same way. It’s impossible to predict how your baby will be affected. The best way you can prepare is to talk to healthcare providers who specialize in researching and treating spina bifida and myelomeningocele.
As they grow, your child may benefit from a team of healthcare providers who can care for their needs.
If your child was born with myelomeningocele, they’ll likely need to see their healthcare provider — or team of healthcare providers — regularly throughout their life.
In particular, it’s important to call your child’s healthcare provider for the following reasons:
If your healthcare provider suspects myelomeningocele, it may be helpful to ask your healthcare provider the following questions:
Learning that your baby has a serious medical condition can feel overwhelming. Know that you’re not alone — many resources are available to help you and your family. It’s important that you speak with a healthcare provider who’s very familiar with myelomeningocele so you can learn more about how your baby will be affected and how to prepare.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.