Asystole is when your heart’s electrical system fails, causing your heart to stop pumping. This is also known as “flat-line” or “flat-lining” because it causes your heart’s electrical activity to look like a flat line on an electrocardiogram. Without immediate CPR or medical care, this condition is deadly within minutes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
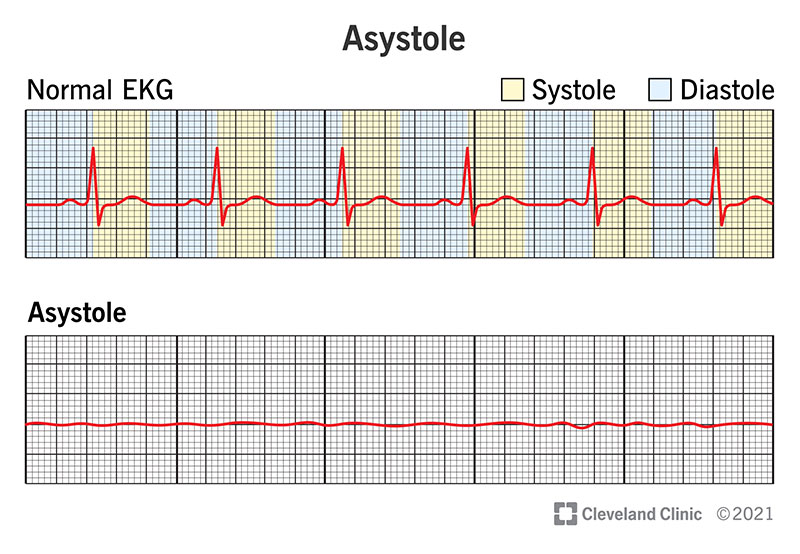
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22920-asystole)
Asystole is when your heart’s electrical system fails entirely, which causes your heart to stop pumping. It is also known as “flat-line” or “flat-lining” because of how your heart’s electrical activity appears as a flat line on an electrocardiogram.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Asystole is a type of cardiac arrest, which is when your heart stops beating entirely. This usually makes you pass out. It’s also likely that you’ll stop breathing or that you’ll only have gasping breaths. Without immediate CPR or medical care, this condition is deadly within minutes.
Asystole is a clinical sign rather than a symptom because you can't see or feel it without special equipment. The only way to “see” asystole is by using an electrocardiogram (often abbreviated as ECG or EKG). This is a diagnostic test that involves several (usually 12) sensors attached to the skin of your chest. Those sensors, called electrodes, detect your heart’s electrical activity and show it as a wave pattern on either a printout or a screen display.
As an electrical current travels through your heart with each heartbeat, an EKG's waves show the strength of that current and how it moves through your heart. There's no electrical activity to create the wave with asystole, so it appears as a flat line.
Every time your heart beats, it does so in two steps: systole (sis-toe-lee) and diastole (dye-ast-oh-lee).
Advertisement
When asystole happens, your heart’s electrical system has no detectable activity at all. Without electrical current, your heart stops pumping entirely, and you go into cardiac arrest. When you go into cardiac arrest, this is a state known as “clinical death.”
From a medical standpoint, death happens in stages. The difference between those stages is whether or not it’s possible to revive someone.
The main types of death here are:
*There are rare cases where a person with brain death will remain on life support machines (usually because a loved one with medical decision-making authority chooses to keep the affected person on life support). However, these people can’t survive without life support. Depending on where this occurs, the law might consider these people legally dead, even if life support keeps their bodies alive.
Because your brain cells can survive without blood flow for approximately five minutes, there may still be a chance to revive you. If healthcare providers can restart your heart quickly enough (and faster is always better), there’s a small chance that you can survive. However, this is not usually the case, and most people don't survive cardiac arrest, especially if it happens outside a hospital environment.
Pulseless electrical activity and asystole are both ways that cardiac arrest happens.
Pulseless electrical activity means that your heart still has electrical activity, but it isn’t strong or organized enough to make your heart pump. On an electrocardiogram, PEA forms wave patterns, some of which look very similar to normal heart rhythms. That means your heart’s electrical system is still working, but it’s too weak or disorganized, and you don’t have a pulse with it. With asystole, you have no pulse and no electrical activity.
Asystole can happen because of any health condition or event that causes cardiac arrest or significantly disrupts your heart’s electrical system. Some of the most common causes of asystole include:
Advertisement
Asystole is part of cardiac arrest, which is a medical emergency where every second counts. While it’s only possible to confirm asystole with an EKG, the treatment for cardiac arrest is the same no matter what the cause.
When cardiac arrest happens outside of a hospital, the most important thing is to immediately start CPR and continue it until emergency medical personnel arrive. Effective, continuous CPR offers the best chance of survival.
Inside a hospital, the following treatments are possible:
Defibrillation is an emergency treatment that involves an intense electrical shock to your chest. It's used to "convert" an abnormal heart rhythm into a normal one. Defibrillation outside a hospital setting is possible using devices called Automated External Defibrillators (AEDs). These devices can detect heart rhythms and deliver a shock if needed.
Advertisement
However, the only “shockable” heart rhythms are ventricular fibrillation and pulseless ventricular tachycardia. Asystole isn't a shockable rhythm, and defibrillation may actually make it harder to restart the heart. Defibrillation is only an option if your heart goes from asystole to a shockable rhythm, which is possible when someone with asystole receives effective CPR.
Asystole, like any form of cardiac arrest, is a medical emergency that needs immediate medical care. If someone near you has the following:
Call 911 (or the appropriate number for your local emergency medical services) and start CPR right away. Immediate, effective, and continuous CPR is critical to saving a person’s life when they are having a cardiac arrest.
If you don't know CPR, calling 911 immediately is still important. That's because 911 dispatchers can give you CPR instructions over the phone, which means you can make a difference and possibly save someone’s life if you don’t know CPR.
Asystole is a dangerous problem that happens with cardiac arrest. Without quick action and CPR, the odds of survival are very low. However, the odds of survival are much higher when a person in cardiac arrest receives CPR quickly and effectively. Knowing how to do CPR and being prepared are critical, and the faster a person with asystole gets medical care, the more likely that they’ll have a good outcome.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
