Acid reflux might happen after a large, rich meal, or when you lie down too soon after dinner. Stomach acid rises into your esophagus, causing heartburn and other symptoms. Occasional acid reflux is manageable at home, but chronic acid reflux (GERD) might need treatment. GERD can damage your esophagus tissues over time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
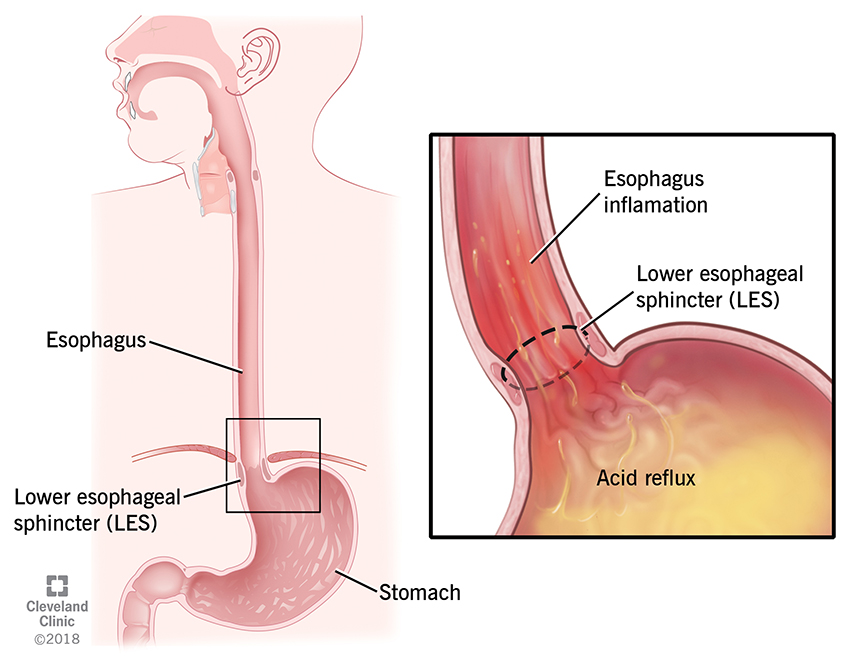
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17019-gerd-chronic-acid-reflux)
Your stomach contents are supposed to travel only one way: down. When acid from inside your stomach flows backward — meaning, up — into your esophagus and throat, it’s called acid reflux.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When acid creeps into places it doesn’t belong, you’re bound to feel it. Acid irritates and inflames the tissues inside your esophagus, which runs from your stomach up through your chest to your throat.
Almost everyone has experienced an occasional episode of acid reflux. It might feel like indigestion — burning stomach pain after eating — or heartburn — burning chest pain close to your sternum.
Occasional acid reflux is uncomfortable, but it’s not a disease. But some people have reflux all the time. Chronic acid reflux can really affect your quality of life, and it can also do real damage to your tissues.
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_6v09sd17/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
What’s the difference between GERD and stomach ulcers?
GERD stands for gastroesophageal reflux disease. Depending on where you live, it may be spelled GORD for gastro-oesophageal reflux disease. However you spell it, GERD is chronic acid reflux in your esophagus. Acid reflux is considered chronic when you’ve had it at least twice a week for several weeks.
Temporary conditions can cause temporary acid reflux. But GERD is a constant, mechanical problem. It means that the mechanisms that are supposed to keep acid out of your esophagus aren’t working right.
Occasional, uncomplicated gastroesophageal reflux (GER) and gastroesophageal reflux disease (GERD) are both common. GERD is estimated to affect about 20% of adults and 10% of children in the U.S.
Advertisement
Symptoms of acid reflux and GERD may include:
GERD symptoms may be worse:
It’s normal for babies to spit up (regurgitate). There might be some acid in it, but usually not enough to really bother them. GERD is a more severe condition that causes distress or complications with feeding.
Babies are more likely to have GERD if they’re born prematurely or with a condition that affects their esophagus. A pediatrician might check for GERD if your baby seems to be struggling in some way.
Symptoms of GERD in babies (or small children) may include:
For acid to get into your esophagus, it needs to get past the valve at the bottom of your esophagus that usually keeps things from coming back up. This valve is called your lower esophageal sphincter (LES).
Your LES is a circular muscle that opens when you swallow and then closes again to keep substances in your stomach. It also opens a little to let gas bubbles out when you’re burping or have hiccups.
Acid reflux happens when your LES weakens or relaxes enough to let acid pass. Some temporary things can relax your LES, like lying down after a large meal. But if you have GERD, it means your LES is relaxing often.
Advertisement
Many things can contribute to weakening your LES, either temporarily or permanently. Sometimes occasional acid reflux turns into chronic GERD when these factors overlap or persist for a long time.
Common causes of acid reflux and GERD include:
Advertisement
Other possible causes of GERD include:
Birth defects. Congenital defects like esophageal atresia and hernias can affect your LES.
Connective tissue diseases. Diseases like scleroderma may affect your esophagus muscles.
Prior surgery. Surgery in your chest or upper abdomen may have injured your esophagus.
Medications. Certain medications can have a relaxing effect on your LES, including:
Foods and drinks probably aren’t enough to cause acid reflux alone, but they can contribute to it. Chocolate, coffee, alcohol, mint, garlic and onions may have a relaxing effect on your LES in higher doses.
Fatty foods increase stomach acid and take longer to digest, so there’s more opportunity for acid to escape. If you have a heavier meal for dinner, it might not have time to digest before you lie down.
Stomach acid is powerful stuff, built to break down the food you eat for digestion. Your stomach has a tough inner lining to protect it from its own acid. But your other organs don’t have this protection.
Advertisement
Acid reflux mostly affects your esophagus, though sometimes it can get into your windpipe or even your airways. A little acid may just feel momentarily uncomfortable. But a lot of acid will injure these organs.
Possible complications include:
A gastroenterologist will evaluate your esophagus to diagnose GERD. Tests may include:
Some people find they can reduce acid reflux with lifestyle adjustments, like changing their eating habits, reducing alcohol and tobacco and losing weight. Healthcare providers encourage this approach.
But if you have chronic acid reflux or GERD, they also recommend medicines to reduce your stomach acid, so reflux is less damaging. These medicines are easily available and highly effective for GERD.
Over-the-counter (OTC) medicines for acid reflux include:
Prescription medications for GERD include:
While medicine can reduce the symptoms and the effects of GERD, it doesn’t stop it from happening. A severe case of GERD may continue to cause complications despite medication, even if you can’t feel it.
When this is the case, you need a more definitive treatment for acid reflux. This usually means a procedure to tighten your LES. These are minor, outpatient procedures, and they’re very effective.
Surgery for GERD includes:
So many things contribute to acid reflux that it can be hard to tell what’s causing yours. Sometimes, simple lifestyle changes can make it go away. But some causes, like a hiatal hernia, may get worse.
If you have mild acid reflux, you can often manage it at home. If you have moderate to severe acid reflux, you might need a prescription to manage it. Medicine works for most people, but not all.
Whether your acid reflux bothers you a lot or a little, it’s a good idea to discuss it with a healthcare provider. They can assess whether it’s causing you complications that you may be unaware of.
If you have severe GERD or it causes complications that medicine can’t help, you might need surgery. But surgery is usually minor and effective. It’s worth treating GERD to prevent its complications.
To help manage acid reflux at home, try:
If it’s happening right now, try:
If you have acid reflux frequently, talk to a healthcare provider. It’s important to find out how it’s affecting your body. GERD isn’t just an inconvenience — it can do real harm. It’s also very treatable.
Almost everyone gets acid reflux from time to time. Heartburn, indigestion and acid regurgitation can make for an unpleasant evening. You can take certain steps to reduce the frequency of these events.
If you have acid reflux often and it significantly affects your life, you might have GERD. It’s worth talking to a healthcare provider about your symptoms. They can assess whether treatment might help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
