“Chronic obstructive pulmonary disease” (COPD) is a term for lung and airway diseases that restrict your breathing. People with COPD have airway inflammation and scarring, damage to the air sacs in their lungs or both. Emphysema and chronic bronchitis are both forms of COPD. Treatments can manage symptoms and reduce exacerbations.
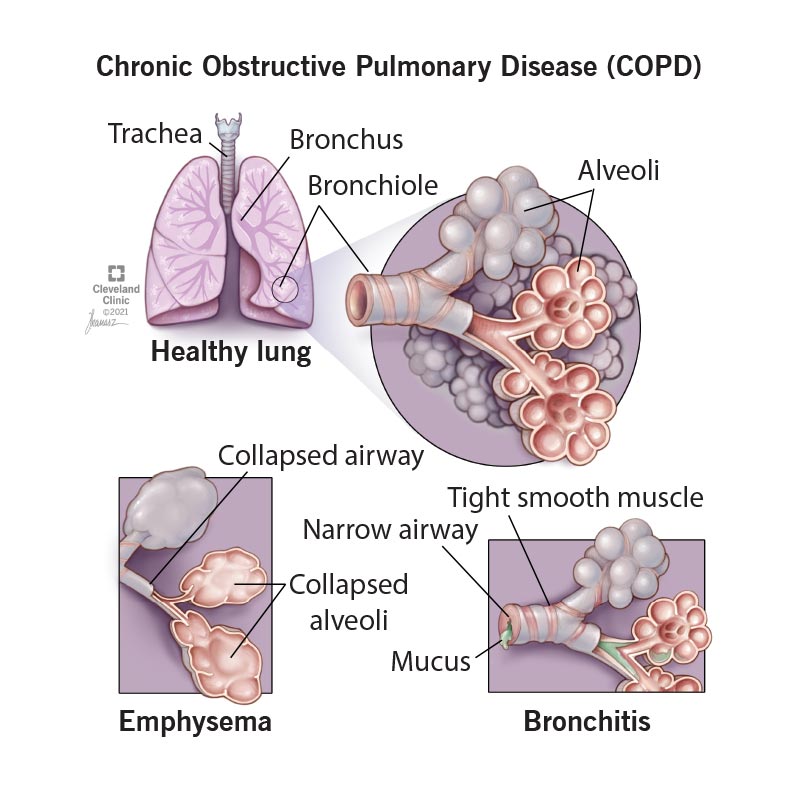
“Chronic obstructive pulmonary disease” (COPD) is a term for certain types of irreversible lung and airway damage that block (obstruct) your airways and make it hard to breathe. If you’re diagnosed with either emphysema or chronic bronchitis, you have COPD.
Changes in your lungs and airways in COPD include:
People with COPD often get exacerbations, or worsening of symptoms, like severe difficulty breathing, thicker mucus, wheezing and cough. You might need to go to the hospital for severe exacerbations.
COPD gets progressively worse over time. Flare-ups get more severe and happen more often. This usually takes years or decades, though some people get worse faster.
COPD includes both emphysema and chronic bronchitis. People with COPD often have features of both.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Symptoms of COPD include:
Damage to your lungs from smoking is the most common cause of COPD. Other causes include:
While smoking is the biggest risk factor for COPD, not everyone who smokes will develop it. You may be at higher risk for COPD if you:
Advertisement
COPD can trap bacteria in your lungs, leading to infections. It can also prevent oxygen from getting into your body and carbon dioxide from getting out. This can lead to serious complications, including:
To diagnose COPD, a provider will perform an exam and ask you about your health history. They’ll test how well your lungs work and might get images of your lungs.
They may ask you questions like:
Your provider might use the following tests to help diagnose COPD:
Advertisement
Your provider can stage COPD based on your forced expiratory volume in one second (FEV1) results. FEV1 is the amount of air you can breathe out in one second, and it can tell your provider how blocked your airways are. Your provider measures FEV1 with spirometry.
COPD stages based on severity are:
Your provider can also evaluate your symptoms and your risk for exacerbation using groupings with the letters A, B and E:
Your stage isn’t directly related to your symptoms — for instance, you could be in stage 3 or 4 but still have mild symptoms. Your provider can use your stage, symptoms and number of exacerbations to guide your treatment.
There’s no cure for COPD. Treatment focuses on improving your symptoms and reducing and treating exacerbations. Your provider may recommend:
The best way to prevent COPD is to avoid smoking and exposure to secondhand smoke and other pollutants that can damage your lungs.
People with COPD are more likely to get respiratory infections, which can lead to pneumonia or cause severe exacerbations of your symptoms. You can reduce your risk of infections by:
The damage to your lungs from COPD is permanent and doesn’t get better. But there are ways to manage your symptoms for a long time, and sometimes even improve them. Following your healthcare provider’s recommendation and a pulmonary rehabilitation program can help improve your symptoms and your quality of life.
How long you live with COPD depends on how severe it is and how quickly it’s progressing. Many people can live for decades after diagnosis, especially with early treatment. People in stage 3 or 4 have a life expectancy that’s six to nine years shorter than average.
COPD gets progressively worse over time, but it’s not always a terminal illness. How quickly it progresses varies from person to person. Over time (usually years or even decades) many people with COPD won’t be able to breathe on their own. But others can live a long time without having severe symptoms.
If you have COPD, some tips to take care of yourself include:
If you think you could have COPD, don’t wait to see a healthcare provider. Early diagnosis and treatment can reduce your risk of your symptoms progressing.
If you have COPD, see your healthcare provider if you have signs of an infection or other changes in your symptoms, including:
Go to the emergency room if you experience:
It might be helpful to ask your healthcare provider:
A note from Cleveland Clinic
Living with chronic lung disease like COPD might feel overwhelming, scary, frustrating or even lonely at times. But there are ways to keep your lung muscles strong for as long as possible and even improve your symptoms. Making a plan with your healthcare team that will keep you healthy and reduce exacerbations can help it feel more manageable. Talk to your loved ones about how they can help, and what to do if you have a flare-up.
If you feel out of breath frequently, have a chronic cough or feel tired easily, don’t wait to talk to a healthcare provider. Early diagnosis can improve your quality of life and help keep you healthy for the years ahead.
Last reviewed on 08/19/2024.
Learn more about our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy