BiPAP® is a type of noninvasive ventilation that helps you breathe. Providers can use it to treat you if you’re not getting enough oxygen or can’t get rid of carbon dioxide. A machine delivers air through a mask on your face. It uses a lower pressure when you’re exhaling than when you’re inhaling.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
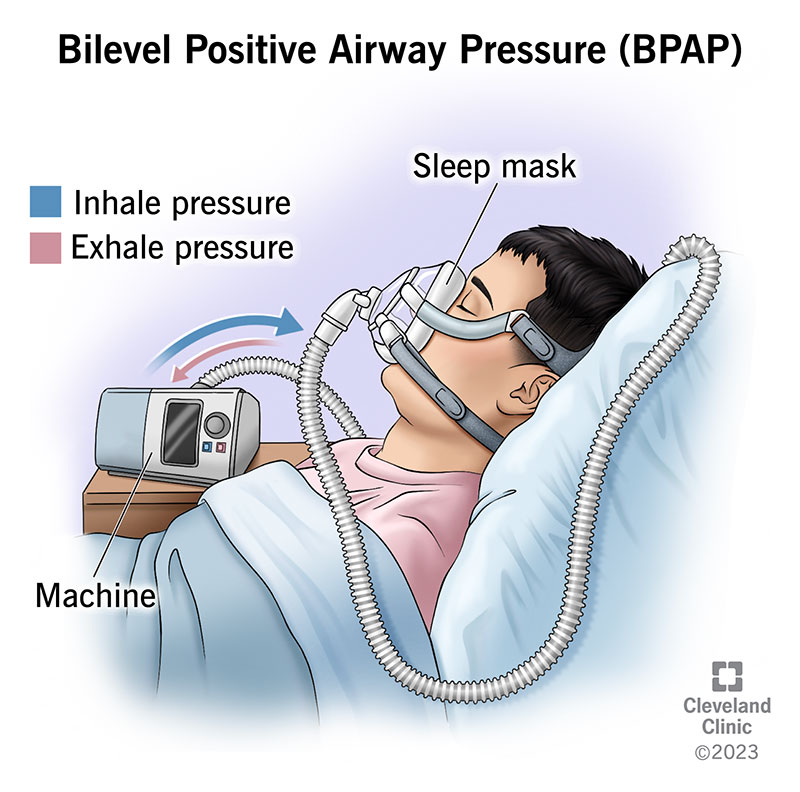
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24970-bipap-machine)
Bilevel positive airway pressure (known as BPAP, or more commonly under the trade name, BiPAP) is a machine that helps you breathe. It’s a form of noninvasive ventilation that providers might use if you can breathe on your own but aren’t getting enough oxygen or can’t get rid of carbon dioxide. Unlike invasive mechanical ventilation, which connects to a tube in your throat, BiPAP delivers air through a mask on your face.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Positive airway pressure” means that the device pushes air at a higher pressure into your airway, which includes your nose, mouth and windpipe (trachea). That higher pressure keeps your airway open and can help move air into and out of your lungs.
“Bilevel” means that it gives you airflow at two different pressures: one for when you’re inhaling and a lower one for when you’re exhaling. These two levels are called inhalation positive airway pressure (IPAP) and exhalation positive airway pressure (EPAP). The machine settings can set the timing of the two pressures (timed) or it can adjust the pressure based on your breathing patterns (automatic).
Providers use BiPAP in certain emergency or intensive care situations. Some people also have a BiPAP machine at home for chronic conditions.
You might use a BiPAP machine if you have certain ongoing conditions or an emergency situation where you need help breathing. Providers can treat the following conditions with BiPAP:
Advertisement
CPAP (continuous positive airway pressure) machines give you the same air pressure whether you’re breathing in or out. BiPAP machines adjust the air pressure you get depending on whether you’re inhaling or exhaling. Most people with sleep apnea use CPAP, but in some situations, your provider may recommend a BiPAP machine.
If a provider is putting you on BiPAP, they’ll:
If you have your own BiPAP, you’ll:
There’s no one answer to this question — how long you’re on BiPAP depends on why you’re on it. Unless you’re treating sleep apnea, most people are only on BiPAP until they can breathe well enough on their own again.
BiPAP isn’t life support and doesn’t take over breathing for you entirely like invasive mechanical ventilation does. If you need to be on BiPAP for more than a few days straight, you need to be able to take breaks. This means either breathing without a machine or getting extra oxygen through a small tube (cannula) just under your nose.
If you’re on BiPAP for sleep apnea, you can use it at night indefinitely.
Benefits of BiPAP include:
Risks and drawbacks of BiPAP include:
Advertisement
How long it’ll take to feel better depends on why you’re on a BiPAP machine. If you’re using it for sleep apnea, it can take a few days to a few weeks to feel better. You may feel more rested, have more energy or notice you don’t need to take a nap during the day. COPD flare-ups can last days or weeks, even with BiPAP treatment.
BiPAP can feel uncomfortable and take some getting used to. If a provider is treating you with BiPAP, they may apply your mask in stages — loosely at first — so that you have time to get used to the feeling. If you’re using BiPAP at home, there are some things you can do to help you adjust:
Advertisement
Talk to your provider if you feel like your sleep apnea or COPD isn’t well managed. They can help you figure out what treatment options might work for your specific condition.
Providers use BiPAP to treat both emergency situations and chronic conditions. The air pressure levels can help some people manage their conditions better. Reach out to your provider if you want to know more about treatment options for your breathing or heart condition. Talk to them about what’s working for you and what’s not. Together, you can make a plan to help you manage your health in a way that works best for you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
