Chronic bronchitis is a form of COPD where your lungs get inflamed and fill with mucus. The most common symptom is a frequent cough that lasts for two years or longer. Chronic bronchitis never really goes away but can be managed with treatment. It’s almost always caused by smoking.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
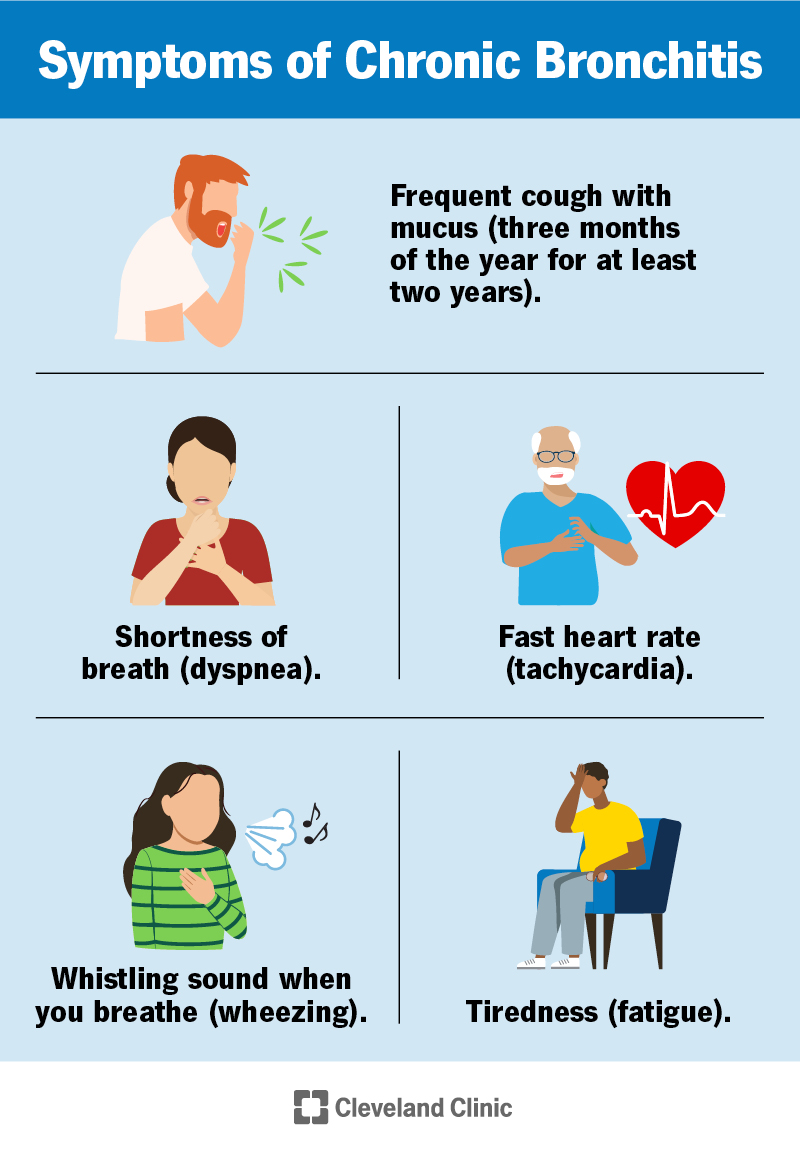
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24645-chronic-bronchitis)
Chronic bronchitis is an inflammation of the airways (trachea, bronchi or bronchioles) in your lungs. People with chronic bronchitis have symptoms like a cough and shortness of breath most days of the month, three months out of the year, for two years or longer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chronic bronchitis is commonly used to refer to chronic obstructive pulmonary disease (COPD). Though you may still hear the term “chronic bronchitis,” it’s now more accurately called COPD. Very few people have chronic bronchitis without the airway blockage (obstruction) of COPD.
Acute bronchitis is usually caused by a virus like the common cold or the flu. It lasts a few days to a few weeks. Chronic bronchitis is when you get symptoms of bronchitis frequently for two years or longer. It’s usually caused by smoking or other lung irritants.
Chronic bronchitis and emphysema are both forms of COPD. They cause similar symptoms but affect different parts of your lungs. Chronic bronchitis causes swelling and mucus in your airways, or tubes, that bring air in and out of your lungs. Emphysema affects the small air sacs at the end of your airways (alveoli) and causes them to collapse. People with COPD often have some damage to both their airways and alveoli.
Chronic bronchitis/COPD often affects people who smoke or used to smoke, but you can also be at risk if you:
Chronic bronchitis is when you have a cough and shortness of breath frequently, caused by damage to your lungs. Irritation in your airways causes an immune system reaction that makes them swell up and fill with mucus.
Advertisement
Usually bronchitis is temporary. But when your airways are often irritated — like from cigarette smoke or breathing in things like dust or smog — it can cause damage that leads to too many mucus-making cells (goblet cells). Additionally, sometimes the tiny, hair-like structures (cilia) that clear mucus out aren’t working properly. This damage makes your airways swell and fill with mucus often. This makes you cough and have trouble breathing.
You’re also more likely to get viral and bacterial infections in your lungs, making your symptoms worse.
The main symptom of chronic bronchitis/COPD is a persistent (stubborn) cough with mucus that happens frequently for at least two years. Other symptoms include:
Smoking is the leading cause of chronic bronchitis/COPD. Pollutants in the air or other lung conditions, like asthma, can also increase your risk. In some cases, you won’t know the cause.
Chronic bronchitis/COPD isn’t contagious. But if you have chronic bronchitis, contagious diseases like a cold or the flu might be more likely to make your symptoms worse (exacerbation).
A healthcare provider will diagnose chronic bronchitis/COPD by determining how well your lungs are working. They’ll ask you about your health history and symptoms and listen to your heart and lungs. They’ll give you lung function tests and might order chest X-rays or other imaging.
Tests for chronic bronchitis/COPD include:
Chronic bronchitis/COPD treatment focuses on managing symptoms. Depending on how severe your symptoms are, your provider might suggest many types of therapy, including:
Advertisement
Healthcare providers call bronchitis “chronic” if you have symptoms at least three months out of the year. Your symptoms may sometimes get better or worse, but — unlike acute bronchitis — chronic bronchitis never fully goes away and may get worse over time.
Chronic bronchitis/COPD can be mild or very serious. It’s usually a sign that you have lung damage that can get worse over time. You can’t cure the damage, but your provider can help you manage your symptoms, slow down its progression and reduce flare-ups. Your provider can tell you what to expect for your specific condition.
Advertisement
Chronic bronchitis/COPD usually can’t be cured, but your symptoms can improve with treatment. Treatment can improve your quality of life and sometimes keep your condition from getting worse.
The best ways to reduce your risk of chronic bronchitis/COPD include:
The best way to take care of yourself is to develop a treatment plan with your provider based on your specific condition. Talk to your provider if you’re using prescribed treatments and therapies as recommended and not seeing improvement.
You can reduce your risk of worsening symptoms (exacerbations) by avoiding getting sick with respiratory illnesses. Getting vaccinated, washing your hands and avoiding large groups of people (especially during cold and flu season) can all help reduce exacerbations and your risk of getting seriously ill.
Talk to a healthcare provider if you think you have chronic bronchitis. Getting on a treatment plan as soon as possible can slow down its progression and improve your quality of life. See a provider if you:
Advertisement
Make sure you understand your treatment plan, how to take any medications and how to use any medical devices (like an inhaler or supplemental oxygen). Other questions you can ask your provider include:
Being diagnosed with a chronic illness like chronic bronchitis/COPD can be daunting. But it’s important to remember that statistics can’t tell you what will happen in your specific situation. Having honest conversations with your provider can give you an idea of what to expect as you manage your illness. There are treatments and education that can help minimize the impact chronic bronchitis has on your life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Chronic obstructive pulmonary disease (COPD) can make every breath you take a huge effort. Cleveland Clinic can help you manage this condition and breathe easier.
