Morning glory syndrome (MGS) is a rare condition that happens when the back of your eye doesn’t develop correctly. Instead of a globe-shaped eyeball all around, the back of your eye has a funnel shape. This increases the risk of vision problems and retinal detachment. MGS isn’t curable, but many of the effects are treatable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
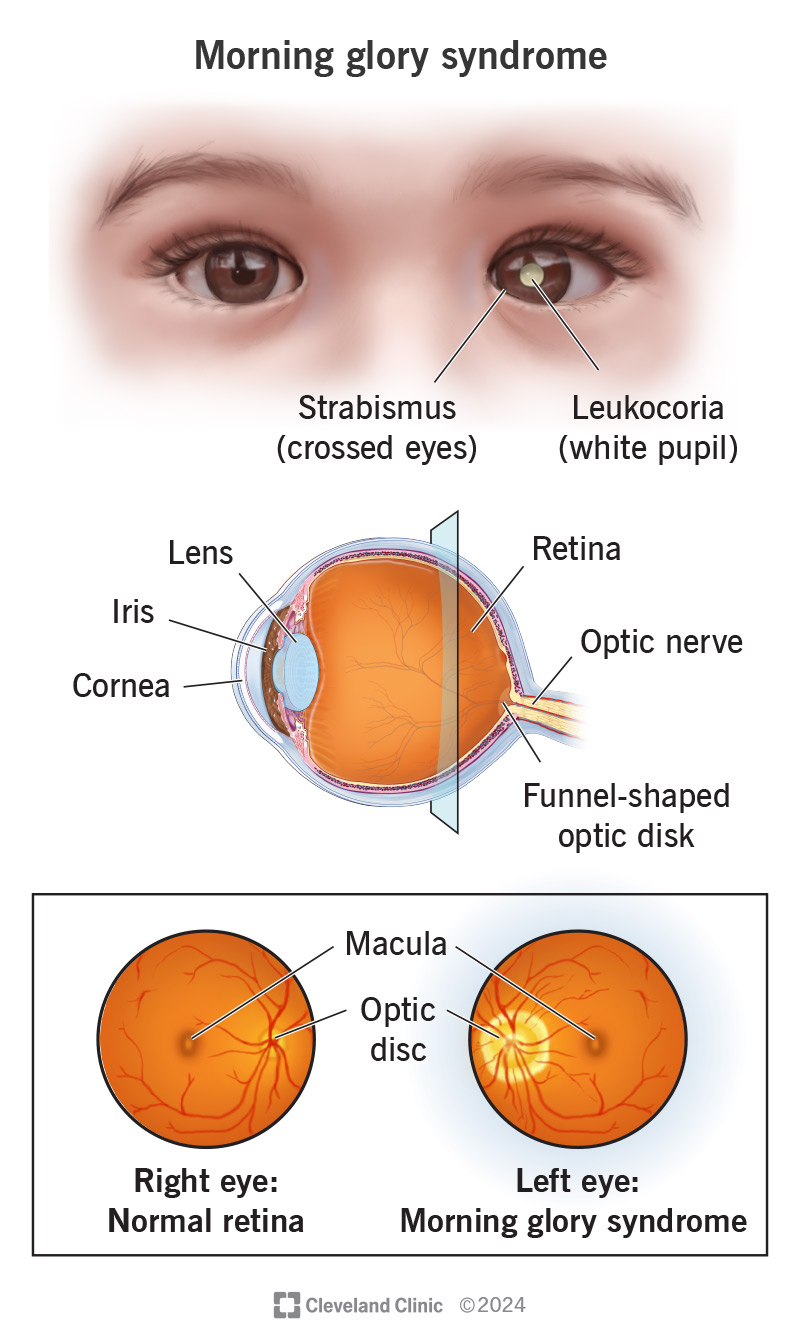
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/morning-glory-syndrome)
Morning glory syndrome (MGS) is a condition where the back of your eye is funnel-shaped because it didn’t develop correctly. Looking into your eye to see your retina is like looking into a morning glory flower, which is why this condition got that name. It happens because of disruptions in your eye development before you are born.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
MGS is almost always diagnosed early in life, often before age 2. The structure differences that MGS causes can disrupt your vision and increase your risk of eye problems throughout your life. It usually happens in just one eye, but it can sometimes happen in both.
Morning glory syndrome is when this happens along with symptoms or other issues. When it happens on its own and the only differences are your eye’s internal appearance and structure — meaning it doesn’t cause symptoms — experts call it morning glory disk anomaly.
Morning glory syndrome is rare. Available data shows it affects a little over 63,000 people under the age of 20 worldwide. It affects females 2:1 compared to males. It’s less likely to affect Black people.
MGS is twice as likely to affect your left eye than your right and can have several symptoms. Not everyone with MGS will have all of them, though. The most common possible symptoms include:
Advertisement
In addition to these symptoms, you might have symptoms from other associated conditions that can happen along with MGS. These include:
Experts aren’t sure exactly how MGS develops. That’s mainly because this is a rare condition and it was only first described in 1969.
But experts do know the cause of MGS has to do with disruptions in eye development that begin before you’re born. These seem to involve the underdevelopment of blood vessels that supply your eyes, or disruptions in eye and optic nerve development.
A key clue that implicates blood vessel problems is that MGS is twice as likely to affect your left eye. A developing fetus normally has small openings between the left and right sides of its heart. Those usually close just before or shortly after birth.
But if a fetus is prone to also developing small blood clots (microemboli), those holes can allow a clot to cross from the left side of its heart to the right. From there, it can go to its brain. If it gets stuck there — which is more likely with disrupted blood vessel formation — it can block blood flow and keep tissue from developing as it should. Cases where this happened helped provide clues that implicate blood vessel development disruptions as a contributing factor to MGS.
While MGS can happen with genetic and inheritable conditions, research doesn’t show that those conditions directly cause MGS. There are records of MGS cases happening to multiple people in the same family, but that isn’t common either.
The most likely complication of MGS is retinal detachment. Nearly 40% of people with MGS will experience this.
Other complications include:
An eye care specialist (especially a retina specialist) can diagnose morning glory syndrome using a combination of methods. That includes learning and asking questions about any symptoms or effects that you notice in yourself or your child.
They’ll also check your (or your child’s) vision and look into the affected eye to see and/or photograph your retina directly. Certain types of retinal imaging scans are also very common and helpful.
Tests that can help with the diagnosis include:
Advertisement
MGS happens because the back of your eye doesn’t develop like it should have. Those development differences aren’t repairable or treatable. That means there’s no way to cure morning glory syndrome or treat it directly.
Instead, treatments focus on the symptoms and complications of MGS. Some of the examples of treatment goals include:
The treatments depend on the specific issue(s) you’re experiencing and many other factors. Your healthcare provider is the best person to tell you about the possible treatments for your specific case and which they recommend.
Most cases of MGS are diagnosed in early childhood. It’s a permanent, lifelong condition. There’s no way to cure, reverse or repair it. It isn’t life-threatening, but it can severely affect your vision. More than one-third of people with MGS will experience a retinal detachment.
Some people with MGS may have “normal” vision (20/20) or near-normal vision (between 20/20 and 20/70), but most won’t. The majority of people with MGS meet the low vision criteria for “partially sighted” (20/70 to 20/200) vision or for “legally blind” (20/200 at most, even with corrections like eyeglasses).
Advertisement
People with one-sided MGS also need to have their unaffected eye monitored closely. That’s because the unaffected eye has a higher risk of certain issues. Retinal detachments are possible because MGS causes nearsightedness, which is a key risk factor for having a retinal detachment regardless of whether you have MGS. The unaffected eye might also have a higher risk of developing cataracts.
Because MGS diagnosis in childhood is so common, parents or caregivers will likely be the ones to make treatment decisions. They’ll also play a key role in watching for signs or behaviors that might indicate their child has a vision issue related to MGS.
Morning glory syndrome isn't preventable, and there’s no way to reduce your risk of developing it.
If you have MGS, the best thing you can do is maintain your eyesight as best you can. Your eye care specialist can guide you on what you need to do to maintain it. It’s important to follow treatment guidelines, use prescription eyewear or other treatments as recommended and see your specialist for regular follow-up visits.
If you have MGS, you have a much higher risk of having a retinal detachment, which is a medical emergency. It’s critical that you get care immediately if you have the symptoms of one. Quick treatment can often prevent permanent damage and restore vision in your affected eye.
Advertisement
The symptoms of a retinal detachment are:
You may want to ask your eye care specialist the following:
If your child or a child you care for has morning glory syndrome (MGS) — a rare condition where the back of their eye doesn’t develop correctly —you might feel worried or frustrated because there’s no way to treat it directly. But while MGS isn’t treatable, many of the issues it causes are.
If your child has MGS, talk to their eye care specialist. There are things you can do to help limit the effects of this condition and keep it from getting worse. Preserving eyesight is a top priority, and advancements in eye surgery and other treatments make this even more possible than in the past.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
