Giant cell arteritis is a kind of vasculitis, which is inflammation of your blood vessels. It’s also known as temporal arteritis. With this type of vasculitis, inflammation causes your large arteries to swell and narrow, which restricts blood flow. The most common symptom of giant cell arteritis is a throbbing headache. Glucocorticoids can help.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
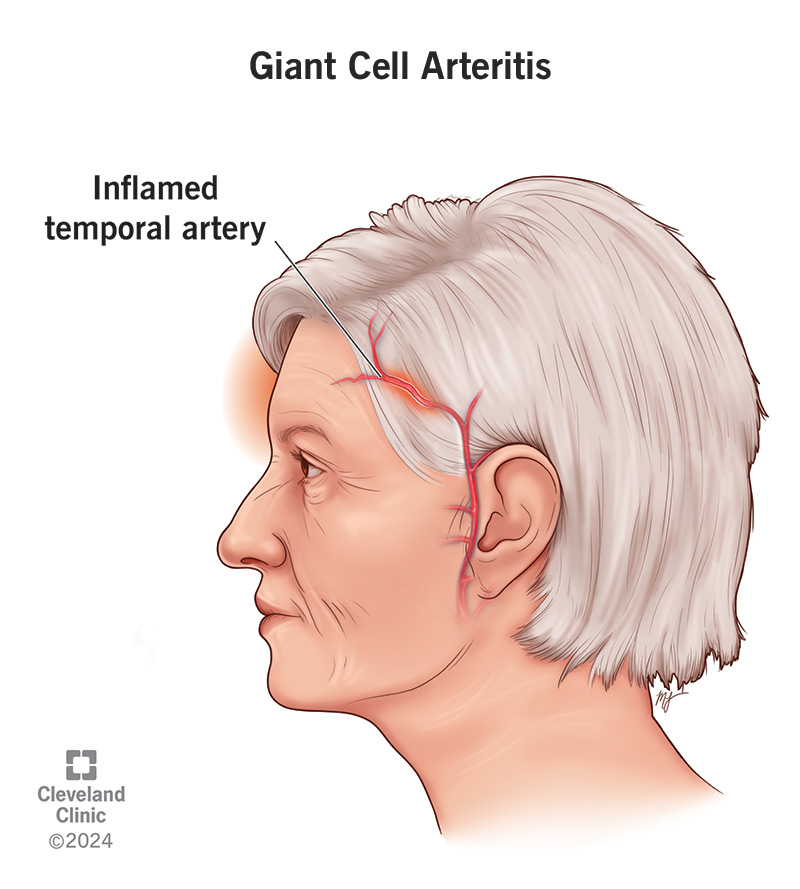
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/giant-cell-arteritis-2)
Giant cell arteritis (GCA), previously known as temporal arteritis, is a form of vasculitis (inflammation of your blood vessels). It affects the large blood vessels in your body, particularly the arteries in your head, neck and arms. These arteries become inflamed, swollen and constricted (narrowed). Inflammation and narrowing of these arteries can interrupt their blood flow, which can damage vital organs and tissues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your temporal arteries, which run along your temples, supply blood to your scalp, jaw muscles and the optic nerve in your eye. When GCA involves these arteries, it can lead to various complications, including blindness. GCA can also involve the largest blood vessels in the body, like your aorta and its branches. Inflammation in your aorta (aortitis) can lead to serious health problems.
Giant cell arteritis commonly occurs together with another inflammatory condition called polymyalgia rheumatica (PMR).
Yes. If not diagnosed and treated quickly, giant cell arteritis can cause:
GCA is one of the most common forms of vasculitis, but it’s a relatively rare condition, affecting about 19-23 out of every 100,000 people in the United States.
The most common symptom of giant cell arteritis is a throbbing, continuous headache on one or both sides of your forehead. Other symptoms may include:
Advertisement
GCA often occurs together with another condition called polymyalgia rheumatica (PMR). This is an inflammatory condition that causes significant stiffness and pain in your shoulders and hips. PMR can occur by itself (and is far more common on its own than GCA is). But up to 40-60% of people with GCA have PMR, and 10-20% of people with isolated PMR, can go on to develop GCA.
Researchers don’t know the exact cause of giant cell arteritis, but many believe it’s an autoimmune or autoinflammatory disease. This means your body’s immune system attacks your healthy blood vessels. Because the condition mainly affects people as they age, some believe it could be linked to the aging process. They also believe genetics and environmental factors that stress your immune system may play a role.
Anyone can get GCA, but it’s most common in:
Your healthcare provider will ask about your medical history and perform a physical examination. They’ll check to see if your pulses are weak in your arms and legs. They’ll also examine your head to look for scalp tenderness or swelling of your temporal arteries.
Your healthcare provider will first order blood tests, like erythrocyte sedimentation rate and C-reactive protein, to measure how much inflammation you have in your body. They may also test for anemia by measuring your hemoglobin levels (the part of your red blood cells that carries oxygen).
If they suspect giant cell (temporal) arteritis, your provider may order a temporal artery ultrasound or temporal artery biopsy. During a biopsy, a skilled healthcare provider removes a small piece of your artery. They send it to a pathologist to examine under a microscope and look for evidence of inflammation (vasculitis).
Other tests that are sometimes necessary include:
Giant cell arteritis treatment should begin immediately to prevent vision loss. The primary treatment is a glucocorticoid, usually prednisone. You’ll likely start taking it at a dose of 40 mg to 60 mg per day (by mouth), and your provider will gradually reduce your dosage. If you already have vision loss or other vision symptoms, your provider may treat you with a high dose of glucocorticoids through a catheter in your vein (IV).
Advertisement
Since glucocorticoids can cause serious side effects, your provider will monitor your response to these medications closely. Because glucocorticoids suppress your immune system, side effects can include more frequent and more severe infections. They can also make your bones thinner, which raises your risk of fractures.
Other side effects may include:
Your provider may want to test your bone density while you’re on glucocorticoids to monitor you for bone thinning. They might recommend treatments to keep your bones strong, like exercises, calcium and vitamin D supplements and possibly medications to prevent osteoporosis.
In 2017, the U.S. Food and Drug Administration approved a new biologic medication called tocilizumab (Actemra®) for the treatment of GCA. This medication is given as an injection (under your skin) or through an IV (in your vein). It can help decrease your need for glucocorticoids. Tocilizumab is associated with other side effects that your provider will discuss with you.
If you’re experiencing symptoms of GCA or infection, or symptoms that are new for you, call your healthcare provider right away. Seeing your provider frequently and getting ongoing lab and imaging tests can help them detect a relapse early.
Advertisement
Questions to ask your healthcare provider include:
Having GCA hasn’t been found to reduce life expectancy, although many different factors can affect this. With early diagnosis and treatment, the outlook is good, and symptoms often start to improve within days.
Without early treatment, the GCA can lead to permanent vision loss, and life-threatening complications, such as aneurysms and stroke. It’s important to see your healthcare provider right away if you experience any of the symptoms associated with GCA.
Once you’ve started treatment, your primary risk is from the side effects of treatment. Also, even with effective treatment and initial improvement, GCA can sometimes return (relapse). Researchers don’t know why relapses occur.
Living with GCA can be challenging. To manage your condition and the side effects that you may experience from glucocorticoids, make sure that you:
Advertisement
There are certain things you should avoid if you have GCA. These include:
Giant cell arteritis (formerly temporal cell arteritis) can be a challenging condition to live with, but people do better when it’s detected early and followed regularly by a skilled practitioner. Symptoms of the condition and side effects of the treatment can take a great toll on your sense of well-being. It can also affect your work and many other aspects of your life. But you don’t have to go through it alone. Ask your healthcare provider to help you find a support group. Sharing stories and tips with others experiencing GCA may help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
