Polymyalgia rheumatica is a condition that causes aches, pain and stiffness in large muscle groups, including your hips and shoulders. The symptoms are usually worse in the morning or after resting. Researchers aren’t sure what causes polymyalgia rheumatica. But it’s treatable. Most people take a corticosteroid to relieve symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
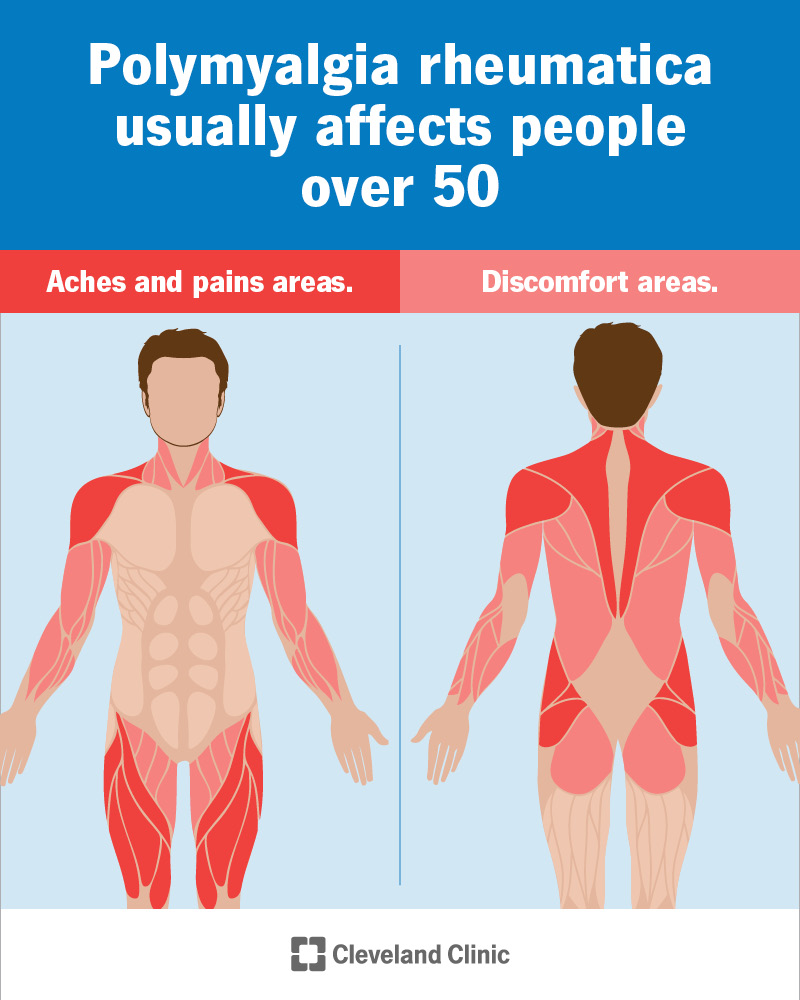
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/polymyalgia-rheumatica-infographic)
Polymyalgia rheumatica (PMR) is a condition that causes pain and stiffness in muscles throughout your body. PMR causes inflammation in your affected muscles. It usually happens in in groups of large muscles, like your:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Polymyalgia rheumatica almost always affects people over 50. But lots of people with PMR assume the symptoms are a normal part of aging. They’re not. It’s true that you might have occasional aches, pains and stiffness as you get older. But you don’t have to live in constant discomfort.
Visit a healthcare provider if you’re feeling any symptoms that make it hard or uncomfortable to move. Or if you have symptoms for more than a few days in a row.
The most common PMR symptoms affect your muscles, including:
You’ll probably have symptoms on both sides of your body at the same time. For example, in both hips or on both sides of your neck. The pain may be bad enough to wake you up at night.
You might notice that pain and stiffness are worse after resting. It’s common to feel them first thing in the morning or right after you’ve been sitting down for a while. They’ll usually last for more than 30 minutes at a time, even after you stand up, stretch and start moving again.
Aches and pains from PMR usually come and go. You might notice them slowly getting worse over a few weeks. At their worst, it can be hard to move and use your body. It might be difficult to do everyday tasks like brushing your hair or getting dressed.
Advertisement
Other signs of polymyalgia rheumatica can include:
PMR symptoms can be hard to pin down. It’s sometimes easy to write them off, especially if they get better and go away. But you know your body better than anyone. There’s a difference between being sore after a weekend of yard work and a more constant issue. Listen to your body and trust your instincts.
Experts don’t know for sure what causes PMR. Some triggers may include:
PMR might be a genetic condition. It sometimes runs in families. It’s possible that parents can pass it to their biological children. Polymyalgia rheumatica has similarities to some autoimmune diseases. Some experts think it might happen when your immune system damages your body instead of protecting it.
Researchers are still studying PMR and its causes. They can’t say for certain why it happens.
You might be more likely to develop PMR if you have a related disease called giant cell arteritis (GCA). This type of vasculitis is another inflammatory condition. It’s common to have GCA and polymyalgia rheumatica at the same time.
Other risk factors can include your:
Untreated polymyalgia rheumatica can make it hard to move. It might be hard to use your affected muscles. This can make it difficult to do all your usual activities. Getting out of bed, getting off the couch or even raising your arms over your shoulders may be difficult.
If you develop giant cell arteritis, you could have a risk of dangerous complications like an aortic aneurysm or vision loss.
It can be tricky for healthcare providers to diagnose PMR. There’s no one test that says for sure you do or don’t have it. Providers can usually diagnose it based on the symptoms you’ve felt, your overall health and how well you respond to treatments.
Your provider will give you a physical exam. Tell them which symptoms you’ve had. Let your provider know if the symptoms change. Or if any activities make them better or worse.
Your provider might order an erythrocyte sedimentation rate (ESR) test. It can’t diagnose PMR. But it can help your provider look for signs of inflammation in your blood. This will help them narrow in on a diagnosis. Having an elevated ESR is common in people who have PMR.
Advertisement
You might need a few imaging tests:
These tests take pictures of your muscles and the tissue around them. They can show inflammation. They’ll also help your provider look for injuries or other issues that can cause similar symptoms. Diagnosing PMR can be part of a differential diagnosis. This is when your provider rules out other, more common conditions before diagnosing you. Other conditions that cause similar symptoms include:
Your provider might give you a low dose of glucocorticoids (steroids). These medicines can treat polymyalgia rheumatica. But they can also help diagnose it. There’s a good chance you have PMR if you feel a lot better within 48 hours after starting a steroid.
Steroids are the most common polymyalgia rheumatica treatment. Especially if a small dose helped your provider diagnose it. They might keep you on the same medicine as a treatment. You might need a daily dose of prednisone.
After a few weeks, your provider will have you take less of the medication. This is called tapering your dose. They’ll continue reducing your dose every month or so. After a year, you might be able to stop the medication. Tell your provider if the symptoms ever come back or get worse. They can always adjust your dose if needed.
Advertisement
Taking steroids can increase your risk of osteoporosis. Your provider might suggest a vitamin D supplement. You may also need a bone density test. They’ll tell you what to expect.
Your provider might suggest other medications too. A medication called sarilumab can help prevent inflammation. It blocks the chemical signals your body reads to cause inflammation in certain areas.
You’ll need follow-up visits with your healthcare provider. They’ll tell you how often they’ll need to check your progress. You may need to visit a rheumatologist. This is a doctor who specializes in treating conditions like PMR.
Even low doses of corticosteroids can cause side effects. Your provider will monitor your body for changes. Let them know if you notice any of the following:
Giant cell arteritis often overlaps with PMR. You may need different treatments for it. Tell your provider if you experience any GCA symptoms, like:
It can be annoying to manage PMR. But it should get better quickly after you start treatment. You might notice that symptoms improve in as quickly as a day or two.
Advertisement
It’s always possible that symptoms will come back. Tell your doctor if you experience them again, especially if it’s the first time in a while.
PMR might get better without treatment. But it can take a long time. Don’t wait to get treatment. Talk to a provider if you’re experiencing any new muscle pain, stiffness or other symptoms.
It’s extremely rare to experience severe complications. PMR usually won’t affect your lifespan.
Untreated PMR can increase your risk of more serious issues like giant cell arteritis and atherosclerosis. These conditions can be fatal, but they’re also treatable.
Low-impact physical activities can help you feel better. They might also reduce how often you experience symptoms. Consider exercises like:
Your provider may suggest physical therapy. A physical therapist will give you exercises that target your affected muscles. This can help strengthen them and relieve symptoms like pain and stiffness.
Researchers don’t know the exact cause of polymyalgia rheumatica, so you can’t prevent the condition.
Polymyalgia rheumatica (PMR) almost always affects people 50 and up. You’ve probably heard jokes about the aches and pains that are just part of life after 50. And yes, everyone has stiff, sore muscles from time to time. But that doesn’t mean you have to live with PMR symptoms forever.
Visit a healthcare provider if you’re experiencing any unusual pain, stiffness or other symptoms. Polymyalgia rheumatica symptoms can be scary. But they’re treatable. And you should start feeling like yourself again very soon after starting treatment.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
