Eosinophilic granulomatosis with polyangiitis (EGPA) is a rare immune disorder involving your respiratory system. It was previously known as Churg-Strauss syndrome. EGPA affects people with a history of allergies or asthma. It causes inflammation in your blood vessels and small masses that infiltrate your tissues, especially in your lungs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
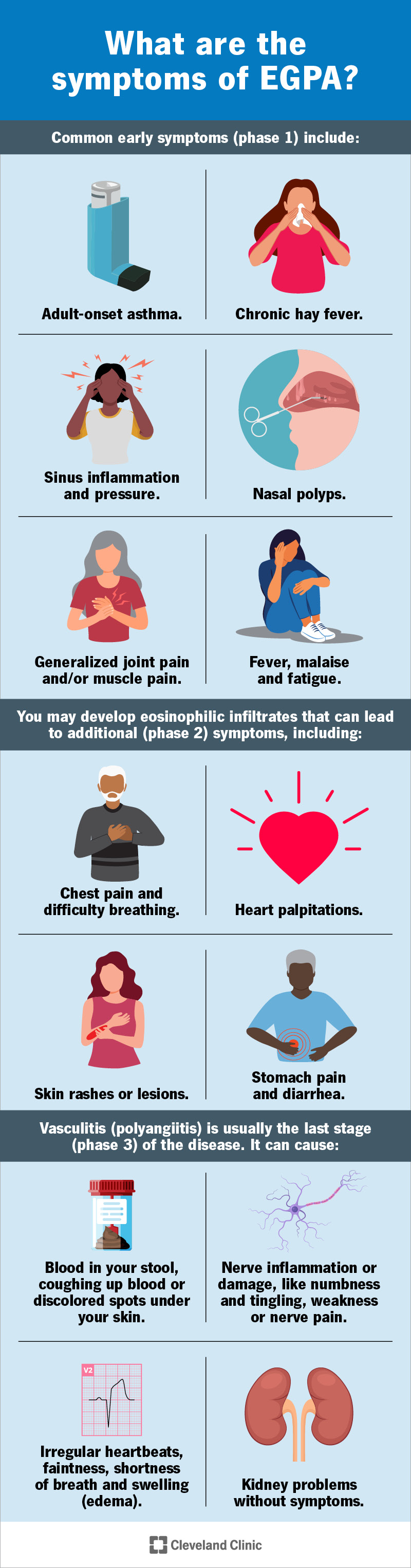
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/churg-strauss-syndrome-egpa-infographic)
EGPA stands for “eosinophilic granulomatosis with polyangiitis.” This is a long name, but it’s more specific than the former name, Churg-Strauss syndrome. EGPA is a rare disorder that occurs in people with a history of severe allergies and/or asthma. It affects your blood vessels, especially the ones in your lungs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Let’s break the name down:
EGPA seems to start with inflammation in your respiratory system, related to allergies or asthma. Eosinophilia and granulomatosis are signs that your immune system is in overdrive. Polyangiitis is a dysfunctional immune response. It’s inflammation that’s automatic, ongoing and has no real target.
Chronic vasculitis weakens the walls of your blood vessels. This can cause them to stretch, leading to an aneurysm, or to break, leading to internal bleeding. Inflammation can also cause swelling and scarring that narrows your blood vessels. This can restrict or stop the blood flow to your tissues and organs.
Advertisement
As your smaller blood vessels travel throughout your body, polyangiitis can cause symptoms throughout your body. But it especially affects the organs that rely on many small blood vessels. EGPA affects your respiratory system the most. It may also affect your kidneys, intestines, heart or nerves.
EGPA develops gradually, and symptoms tend to occur in phases over several years.
Common early symptoms (phase 1) include:
As the condition progresses, you may develop eosinophilic infiltrates — clusters or masses of eosinophils that infiltrate your lungs and other tissues. This can lead to additional (phase 2) symptoms, including:
Vasculitis (polyangiitis) is usually the last stage (phase 3) of the disease. It can cause:
Polyangiitis will often affect your kidneys as well, but usually without symptoms.
Eosinophilic polyangiitis with granulomatosis (EGPA) develops from an overreaction from your immune system. Your immune system generates the inflammation in your blood vessels, the granulomas in your tissues and the eosinophilia that cause your symptoms. But researchers aren't sure why this happens.
Diseases that involve chronic inflammation from your immune system are sometimes called autoimmune diseases. One common feature of autoimmune diseases is that your body can develop antibodies that target certain cells in your body with inflammation. This may be one factor in EGPA.
Researchers have grouped EGPA together with a handful of similar conditions that all involve a certain autoimmune antibody, called ANCA. They call these conditions ANCA-associated vasculitis, or AAV. However, only about 40% of people with EGPA have the ANCA antibody, so it’s not the only factor.
Advertisement
Eosinophilia seems to be a separate cause of symptoms that often occur long before vasculitis does. When eosinophils accumulate in your tissues, they trigger inflammation and damage them. Eosinophilia is related to asthma and allergies. People with asthma are 34 times more at risk of EGPA than others.
If it goes untreated, EGPA can cause serious damage to your organs and tissues, including:
EGPA can be tricky to diagnose. You might have different symptoms at different times, and you and your healthcare provider might not connect them all together right away. Symptoms of EGPA can also resemble many other conditions. Your provider might suspect EGPA if you have most of these:
Treatment for EGPA begins with a high dose of corticosteroids to reduce inflammation and eosinophils. When they’ve reduced enough to relieve your symptoms, your disease is in remission. At this point, your provider will begin reducing your dose. Most people continue to take a low dose of corticosteroids to maintain remission.
Advertisement
Your provider may prescribe additional medications if corticosteroids alone aren’t effective enough, or if you want to avoid taking a high dose of corticosteroids.
Additional medications include immunosuppressants and biologics. Mepolizumab is the first U.S. Food and Drug Administration (FDA)-approved biologic therapy for EGPA. Benralizumbab, another biologic agent, performed equally well in a recent clinical trial. These recent breakthroughs in research offer new treatment options for people with EGPA.
EGPA is treatable, but not curable. Most people can manage their symptoms with medications and even achieve remission, meaning symptoms go away. But when you stop treatment, symptoms may start again (relapse). Your healthcare provider will continue to monitor your condition throughout your life.
With effective treatment, you can have a normal life expectancy with EGPA. In the advanced stages of the disease, complications like organ failure can affect your life expectancy. But treatment can often stop or reverse organ failure. With treatment, EGPA survival rates after five years are over 80%.
As we don’t know what causes EGPA, we don’t know any way to prevent it. However, recognizing it and treating it earlier can prevent it from worsening. By paying close attention to your symptoms and reporting them to your healthcare provider, you may be able to prevent the complications of EGPA.
Advertisement
Medications for EGPA reduce your immunity, which makes it easier for you to get sick and harder for you to get better. When you’re taking these medications, you’ll need to take extra care to protect yourself from common illnesses, because you won’t be able to “bounce back” as easily as before.
Long-term treatment with corticosteroids can also cause side effects, including high blood sugar and weight gain, bone thinning and mood changes. Your provider will work with you to manage side effects while managing EGPA. Stay in touch with your provider about all your symptoms, especially new ones.
Eosinophilic granulomatosis with polyangiitis (EGPA) is one of the rarest types of vasculitis, and one of the trickiest to diagnose. You may have a variety of symptoms that seem unrelated to each other, and it may take time for your provider to figure out what they mean and what treatment you need.
Fortunately, treatment can effectively suppress EGPA. But you’ll have to make some changes to the way you live day-to-day. It might feel lonely at times to live with a chronic disease that most people have never heard of. You might find it helpful to reach out to support networks of others living with EPGA.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
