Auto-brewery syndrome causes symptoms of intoxication in people who haven’t consumed any alcohol. In this rare phenomenon, yeasts that normally live in your gut become overgrown. When they feed on the sugars you eat, they produce alcohol through fermentation. Treatment involves antifungals and eating fewer carbohydrates.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Auto-brewery syndrome (ABS) is a rare condition that causes alcohol intoxication in people who haven’t consumed any alcohol. It’s also known as gut fermentation syndrome (GFS). It happens when microbes in your intestines ferment the sugars that you eat to produce ethanol — just like a brewery in your gut.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
We all have microbes living in our guts, usually harmlessly. Alcohol-producing bacteria and fungi like Saccharomyces cerevisiae (brewer’s yeast) are part of a normal gut microbiome. They also produce small amounts of ethanol in all of us. A normal metabolism usually clears it before it reaches our bloodstream.
In auto-brewery syndrome, these microbes produce ethanol at a rate that exceeds your body’s capacity to clear it. The excess alcohol in your bloodstream causes your blood alcohol content (BAC) to rise to intoxication levels. Yeast overgrowth, high blood sugar and impaired metabolism can all contribute.
There are fewer than a hundred documented cases of auto-brewery syndrome, but most researchers suspect it’s more common than we know. Low awareness of the condition makes it hard for people and their healthcare providers to recognize it. It can also be difficult to diagnose when they do suspect it.
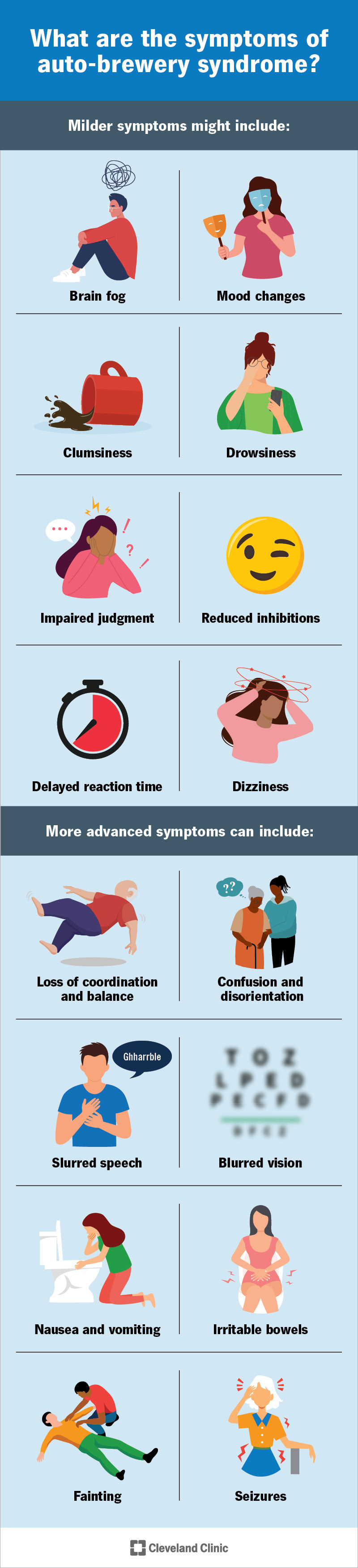
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/auto-brewery-syndrome.jpg)
Auto-brewery syndrome causes alcohol intoxication, just like drinking alcohol does. If you’ve ever experienced this or witnessed it, you might recognize the symptoms. The symptoms are subtler at lower levels. But as blood alcohol content (BAC) rises, they’ll more closely resemble what we know as “drunkenness.”
Advertisement
Milder symptoms might include:
More advanced symptoms can include:
When you’re not intoxicated, you might have other symptoms, like:
Symptoms of intoxication tend to follow meals and drinks high in carbohydrates, like pasta, potatoes and fruit juice. The process can take up to 24 hours. If you’re not aware of how this works, symptoms will seem to occur randomly. They can interfere with important social events and activities like driving.
Auto-brewery syndrome happens when microbes living in your gut ferment the carbohydrates passing through it and produce ethanol — so much that it intoxicates your bloodstream, making you “drunk.” For this to occur, one or several things in your digestive system are out of balance or not working right:
A healthy gut microbiome supports many different types of microorganisms — most of which are harmless, and many of which are helpful to us. The variety of microbes in your gut helps prevent any one type from overgrowing. But certain conditions can throw this balance off. This is called dysbiosis.
In auto-brewery syndrome, an overgrowth of gram-negative bacteria or yeasts like Saccharomyces cerevisiae or Candida albicans causes an excess of fermentation in your gut. Many different factors can contribute to gut dysbiosis, but the most significant ones are medications and medical conditions.
Contributing factors may include:
Even normal, healthy guts produce small amounts of fermentation and alcohol (endogenous ethanol). But not much of it will ever reach your bloodstream. That’s because your liver takes the first pass at metabolizing the alcohol in your gut before the leftovers begin to accumulate in your blood.
But certain conditions can affect this first-pass metabolism. Some people have a genetic variation that impairs one of the enzymes you need to metabolize alcohol in your liver. Advanced liver disease can also impair your liver’s ability to metabolize alcohol. These conditions can sometimes contribute to ABS.
Advertisement
You might be more likely to develop auto-brewery syndrome if you have or have had:
Auto-brewery syndrome affects your body, brain and life just the way frequent alcohol use would. The potential complications are the same as those for alcohol use disorder. Besides interfering with your relationships and job performance, frequent intoxication will affect your mental and physical health.
Complications can include:
Alcohol intoxication can be life-threatening at higher levels, when it becomes alcohol poisoning. This usually occurs at BAC levels over 0.30. Auto-brewery syndrome can cause these levels of intoxication, though it’s unlikely. Alcohol poisoning is more of a risk for children and people with lower tolerance.
A healthcare provider might suspect auto-brewery syndrome if you:
Advertisement
They’ll confirm these things through observation, discussion and testing. They’ll ask about your eating and drinking habits, then observe your symptoms and test them repeatedly over a period of time.
Tests might include:
First-line treatment for auto-brewery syndrome focuses on restoring balance to your gut microbiome. Your healthcare provider will prescribe antibiotics or antifungals to target the overgrowth. Then, they’ll review your diet, reduce carbohydrates and sometimes make other personalized recommendations.
This approach works for most people. But some people with severe dysbiosis might have a harder time rebooting their gut microbiomes. They might need a little extra support, like a personalized nutrition plan, targeted probiotics or treatment for other conditions contributing to auto-brewery syndrome.
The treatment approach to auto-brewery syndrome is simple and straightforward, and it’s usually successful. But some people do have a harder time fixing it than others. Treatment also won’t necessarily cure ABS forever. If the conditions that caused it become active again, ABS could return.
Advertisement
If you have one or more of the risk factors — conditions that raise your risk of developing auto-brewery syndrome — you might want to take extra care of your gut health to help prevent dysbiosis. This begins with eating a good variety of plants and other whole foods, and reducing sweets and starches.
You can also make a point of adding probiotic and prebiotic foods to your diet to boost your gut flora, or ask your healthcare provider to recommend a good probiotic supplement. This is especially important if you’ve recently taken antibiotics or other medications that may have depleted your gut microbiome.
While living with and recovering from auto-brewery syndrome, your healthcare provider will advise you to cut back on carbohydrates (sugars and starches). These are the foods that feed the yeasts in your gut and provide fuel for fermentation. Reducing them will reduce fermentation and your yeast population.
Foods to avoid include:
If you don’t know when symptoms of intoxication are going to pop up, you probably shouldn’t drive. But if you’re aware of your condition and how your eating habits affect it, you might be able to predict the cycle and schedule your driving around it. Hopefully, treatment will eventually make this unnecessary.
This lesser-known variation of auto-brewery syndrome occurs in your bladder instead of in your gut. It’s also called bladder fermentation syndrome. In urinary ABS, fungal overgrowth in your urinary system feeds on excess sugars in your urine, producing alcohol in your pee that passes to your bloodstream.
Auto-brewery syndrome is rare, but gut dysbiosis isn’t. Between our highly processed, highly sweetened Standard American Diet and the continuing rise of metabolic diseases, not all of us have a thriving gut microbiome to start with. A simple event, like an illness, might be enough to tip the scales to dysbiosis.
This happens gradually, but you’re likely to notice symptoms along the way. If your digestive system starts to complain on a regular basis, take notice. Our guts can be sensitive, but they’re also resilient. Simple lifestyle adjustments are often enough to restore health and variety to your gut microbiome.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
