Alcohol-associated liver disease happens after years of heavy alcohol drinking. It causes toxic fat to build up in your liver, which leads to inflammation and scarring (cirrhosis). Most often, there are no symptoms. Treatment is limiting or quitting alcohol use. Your doctor can help you understand how damaged your liver is.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
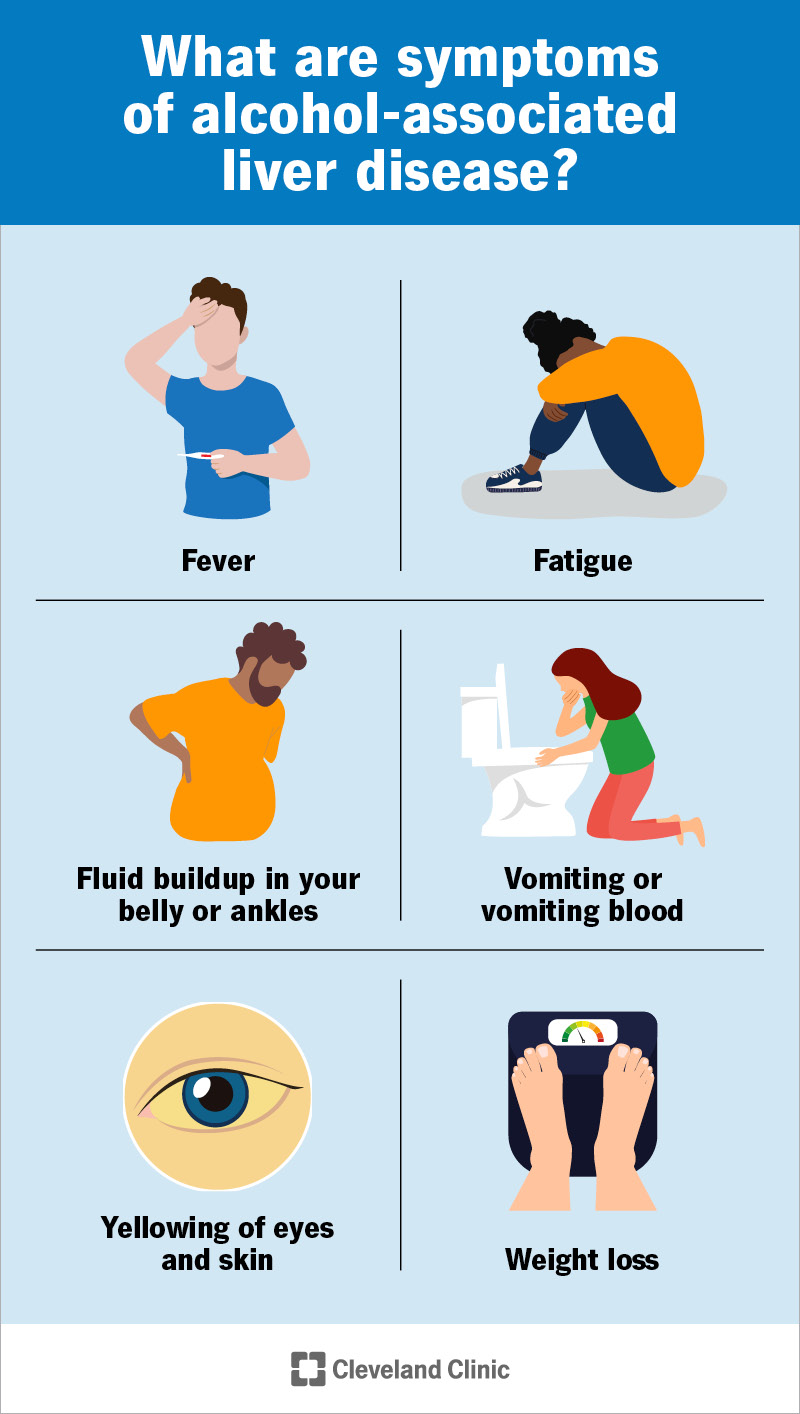
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/alcohol-associated-liver-disease.jpg)
Alcohol-associated liver disease (ALD) is what happens when frequent, heavy alcohol use does long-term damage to your liver. Healthcare providers previously referred to this as alcoholic liver disease. It’s one of the most common causes of chronic liver disease, which can progress to cirrhosis and liver failure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Alcohol-associated liver disease progresses in stages:
When too much of your liver tissue is damaged, your liver functions start to fail (liver failure).
The term “alcoholic liver disease” suggests that the disease comes from alcohol dependency or alcohol use disorder — what we used to call “alcoholism”. But that’s not entirely accurate. Alcohol-associated liver disease comes from heavy alcohol use — whether you have a dependency on alcohol or not.
Healthcare providers changed the name to make this clear. They use the term alcohol-associated liver disease (or alcohol-related liver disease) because alcohol is the cause, not alcohol dependency.
Advertisement
You can have liver disease without symptoms. Often, fatigue is the first symptom.
Later, you may have:
Alcohol-associated liver disease develops when you drink so much alcohol that it affects your liver function. Alcohol is a toxin, and it’s your liver’s job to process it. If it has too much to process, it affects your liver’s other jobs — like processing fats. This causes fat to start building up in your liver.
Most people who have alcohol-associated liver disease develop it after five to 10 years of heavy alcohol use. The definition of heavy alcohol use differs depending on sex:
Research shows 90% of people who drink this much alcohol develop steatosis — the first stage of alcohol-associated liver disease. As fat builds up in your liver, it triggers inflammation (hepatitis), which leads to scarring and, eventually, cirrhosis. About 30% of people reach this stage.
How much and how often you drink alcohol are the most important risk factors in developing ALD. So, your risk is higher if you have alcohol use disorder or engage in routine binge drinking. Alcohol may also do more damage to your liver if you have another liver disease at the same time — like hepatitis C.
If liver disease advances to cirrhosis, it can lead to life-threatening complications like:
A healthcare provider will examine you and ask about your health history. They may ask how much alcohol you drink. That question may make you feel uncomfortable. You may be reluctant to discuss your drinking habits. But understanding how much alcohol you drink helps your provider make the right diagnosis.
You may have tests like:
Some blood alcohol biomarkers can show heavy alcohol use up to months after you use alcohol.
Advertisement
Quitting alcohol is the most important treatment for alcohol-associated liver disease. If you’re still in the early stages of liver disease, quitting can give your liver a chance to recover and repair the damage. This may sound simple — but for some people, it isn’t. If you have alcohol use disorder, your provider might recommend:
If you have cirrhosis, the damage to your liver is no longer reversible. At this stage, a liver transplant is the only cure. If this is a safe option for you, you’ll join a national waiting list to get a liver transplant.
You may want to talk to a provider if you think you’re drinking too much alcohol too often. Your provider knows it’s not always easy to share personal information like alcohol use. They’ll discuss your concerns without making judgments and check your health to see how alcohol use is affecting your body.
You might want to ask your provider:
Advertisement
Your prognosis (outlook) will depend on the stage of your liver disease and whether you stop drinking alcohol. If you’re still in the early stages, you can stop the process and reverse the damage. Steatosis — fat storage in your liver — may stop in as little as six weeks. This allows the inflammation and scarring to stop.
Things are different if you have cirrhosis. That means there’s too much scarring in your liver to undo. Quitting alcohol can keep it from getting worse, but it won’t get better without a liver transplant.
These factors also affect your life expectancy. If you stop drinking alcohol in the early stages of liver disease and your liver recovers, your life expectancy may be normal. Once you have cirrhosis, your life expectancy is generally two to 15 years from diagnosis. Getting a liver transplant could change this.
It can be hard to acknowledge that you regularly drink a lot of alcohol. It can be harder to tell a healthcare provider how much and how often you drink. But sharing that information is important. It’s how a provider may diagnose alcohol-associated liver disease.
Early diagnosis and treatment are key to stopping the progression of liver disease. Your provider knows quitting alcohol is hard to do. They’re here to help you, not to judge you. The first step toward getting well starts with being open about your alcohol use.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic providers compassionately diagnose and treat all liver diseases using advanced therapies backed by the latest research.
