IgA nephropathy, or Berger’s disease, is a kidney disease in which IgA antibodies build up abnormally. Over time, it leads to kidney damage or kidney failure. Symptoms include blood in your pee, swelling and flank pain. Medications can slow the disease’s progress. But some people may need dialysis or a kidney transplant.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
IgA nephropathy (nuh-FROP-uh-thee) is a type of kidney disease. In people with IgA nephropathy, antibodies build up in their kidneys and cause inflammation. The inflammation damages their glomeruli (glo-MARE-yoo-lye). Glomeruli are tiny blood vessels that perform the first step in filtering waste products out of your blood, which eventually leave your body in your urine (pee). Glomerular diseases cause your kidneys to leak blood (hematuria) and protein (proteinuria) into your pee.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Other names for IgA nephropathy include:
Another common name for IgA nephropathy is Berger’s disease. Two French doctors, Jean Berger and Nicole Hinglais, discovered IgA nephropathy in the late 1960s.
IgA nephropathy is a big term. But what does it mean?
Without treatment, IgA nephropathy may gradually get worse and cause kidney failure (renal failure). Kidney failure is fatal without treatment.
IgA nephropathy is a common kidney disease that can happen to people at any age.
In the United States, about 1 out of every 10 kidney biopsies show IgA nephropathy. In East Asian countries, IgA nephropathy appears in about 4 out of every 10 kidney biopsies. In European countries, it appears in between 2 and 3 out of every 10 kidney biopsies.
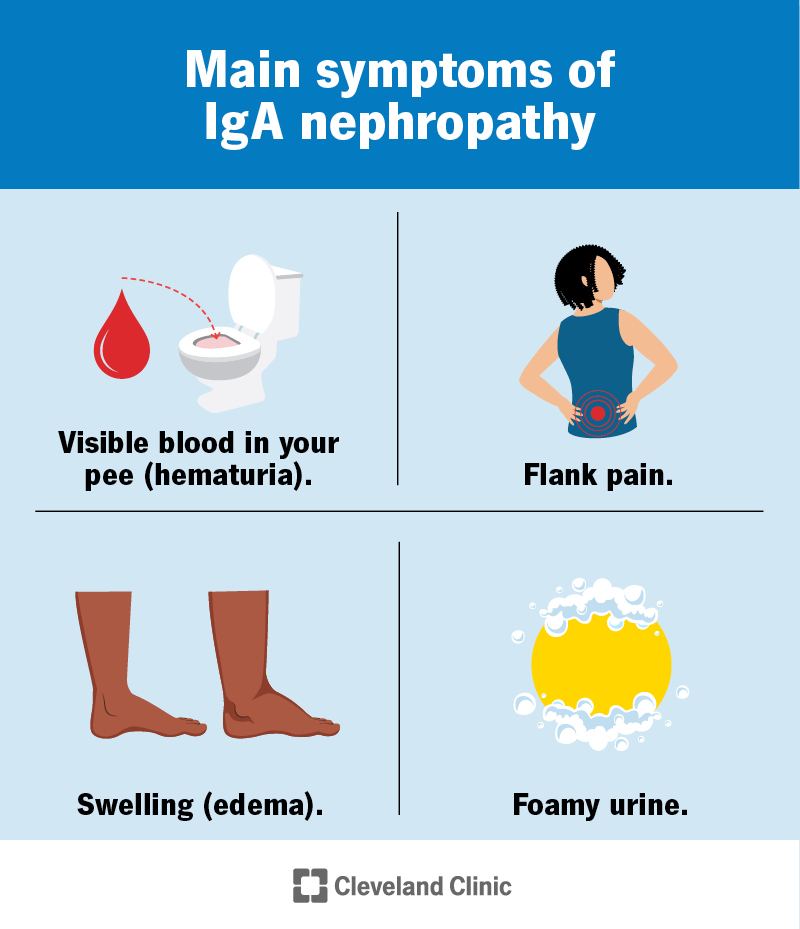
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/iga-nephropathy)
The most common IgA nephropathy symptoms include:
Advertisement
You may not have any IgA nephropathy symptoms at first. It can be years or even decades before signs appear.
Medical experts believe IgA nephropathy is an autoimmune disease. That means your immune system attacks your kidneys.
People with IgA nephropathy have a higher level of IgA with less galactose (guh-LAK-tohs) than is typical. Galactose is a type of sugar. Your immune system considers these low-galactose IgA to be foreign invaders. As a result:
IgA immune complexes circulate in your body more when you have a cold or upper respiratory infection. Some of these complexes end up in your kidneys. As a result, some people have symptoms of IgA nephropathy after a cold.
For some people, there’s a genetic family history of IgA nephropathy. Medical experts have discovered some genetic markers. That means there may be a link between a genetic variation and IgA nephropathy.
Risk factors for IgA nephropathy include a genetic family history of:
Although IgA can affect anyone, you may be more likely to have it if you’re:
In the U.S., males are twice as likely to have IgA nephropathy as females.
IgA nephropathy can affect anyone at any age. But the first signs of the disease usually occur in a person’s late teens to late 30s.
IgA nephropathy complications may include:
Your healthcare provider will ask about your symptoms and medical and family history. You may have:
If you need further testing, your healthcare provider may order a kidney biopsy. This procedure can confirm a diagnosis of IgA nephropathy.
Advertisement
Your healthcare provider uses a needle to remove a small piece of kidney tissue. A pathologist examines the tissue to look for IgA deposits in the glomeruli and see the extent of the damage.
Treatment can slow the progress of the disease and prevent ESRD. If you have IgA nephropathy, your healthcare provider will probably refer you to a nephrologist, a kidney disease specialist.
Treatment for IgA nephropathy includes medication to:
Some research shows that a tonsillectomy (tonsil removal) can benefit a small portion of people who have IgA nephropathy. Talk to your healthcare provider to see if this may be an option for you.
It depends. Sometimes, IgA nephropathy gets better with conservative treatment. In rare cases, IgA nephropathy progresses rapidly. Kidney failure can develop within a few years.
With the right treatment, many people can keep their kidneys as healthy as possible and slow the disease’s progression.
Advertisement
About 1 in 4 adults with IgA nephropathy eventually develop kidney failure. About 1 in every 10 to 20 children with IgA nephropathy develop kidney failure.
It depends. Everyone’s disease progression is different. Some people respond well to treatment and can live with the condition for a long time.
If IgA nephropathy progresses to kidney failure, you may need to consider dialysis or a kidney transplant. Your care team will discuss your treatment options with you.
IgA nephropathy is typically a lifelong, progressive kidney disease. That means it usually gets worse as time goes on. But medications can help slow the condition’s progression.
A 2017 study of adults with IgA nephropathy in the southeastern U.S. found that life expectancy is reduced by a little over 10 years. The average age of death was just under 66 years, while the expected age of death if you don’t have kidney disease was just under 76 years.
A 2019 study in Sweden found that life expectancy is reduced by about 6 years.
With proper treatment, many people with IgA nephropathy can live long, fulfilling lives. They can continue working, going to school and participating in activities they love.
There isn’t a known way to prevent IgA nephropathy. If IgA nephropathy runs in your family, talk to your healthcare provider. They can recommend steps to stay healthy, such as keeping blood pressure and cholesterol well managed.
Advertisement
Researchers have not found a link between nutrition or eating habits and preventing IgA nephropathy.
Some healthcare providers may recommend diet restrictions if you have IgA nephropathy. This may include cutting back on:
A provider may also advise you to avoid foods high in saturated fat and cholesterol if you have high cholesterol.
Proteins break down into products that your kidneys need to filter. Eating too much protein may overwork your kidneys and cause them to decline faster. However, if you don’t eat enough protein, you may develop malnutrition. A healthcare provider may recommend that you see a renal (kidney) dietitian to develop kidney-friendly eating patterns.
If you’re supposed to cut back on how much protein you eat, you may need regular blood tests to check your protein levels.
If you have IgA nephropathy, some healthcare providers may recommend fish oil supplements that contain omega-3 fatty acids. They may lower blood pressure and slow the progress of the disease.
It’s important to talk to a healthcare provider before you start taking any supplements, including fish oil.
It’s a good idea to schedule regular wellness checkups with a healthcare provider. Early detection can help prevent IgA nephropathy from developing into kidney failure. You should also work with a provider to help manage any other conditions that can affect your kidneys, including high blood pressure and diabetes.
Go to the nearest emergency room if you have IgA nephropathy and develop symptoms of kidney failure, including:
You may wish to ask:
Hearing you have a kidney disease can be a big shock. Information can come at you fast, on top of scheduling more tests or making appointments with specialists. It’s important to take a breath so you can process the news and learn about IgA nephropathy.
Some cases are mild — you may need conservative treatment and regular testing to monitor your kidney function. Others are more serious and require medications to help preserve kidney function. But remember that managing IgA nephropathy is possible, and many people can live for years with proper treatment.
Lean on your trusted family members and friends for help. Support groups can also help you confidentially share your feelings and experiences. And if you have any questions, don’t hesitate to reach out to a healthcare provider.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have a condition that’s affecting your kidneys, you want experts by your side. At Cleveland Clinic, we’ll work with you to craft a personalized treatment plan.
