Henoch-Schönlein purpura (HSP) is a type of vasculitis that causes a distinctive reddish-purple rash on your child’s skin. The rash may occasionally itch but doesn’t hurt. The condition causes other uncomfortable symptoms. Fortunately, the symptoms usually go away on their own within a few months. HSP may also be known as IgA vasculitis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Henoch-Schönlein purpura (HSP) is a type of vasculitis. Vasculitis is a condition that causes irritation and swelling in your blood vessels. In the HSP form of vasculitis, the swelling usually affects the small blood vessels in your skin. But it can also affect your kidneys, intestines and joints.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
HSP occurs when an antibody in your immune system called immunoglobulin A builds up in your blood vessels. This buildup causes your blood vessels to burst and leak blood under your skin. This leads most people to develop a spotty, purplish skin rash that looks like small bruises or pools of blood.
HSP is a clinical form of immunoglobulin A vasculitis (IgA vasculitis). Healthcare providers name it after the antibody that causes it. The condition can affect anyone. But it most often affects children.
IgA vasculitis usually isn’t serious. Most children recover from it on their own without treatment. Henoch-Schönlein purpura in adults can be more severe. If it affects your kidneys, you may need treatment to prevent long-term complications.
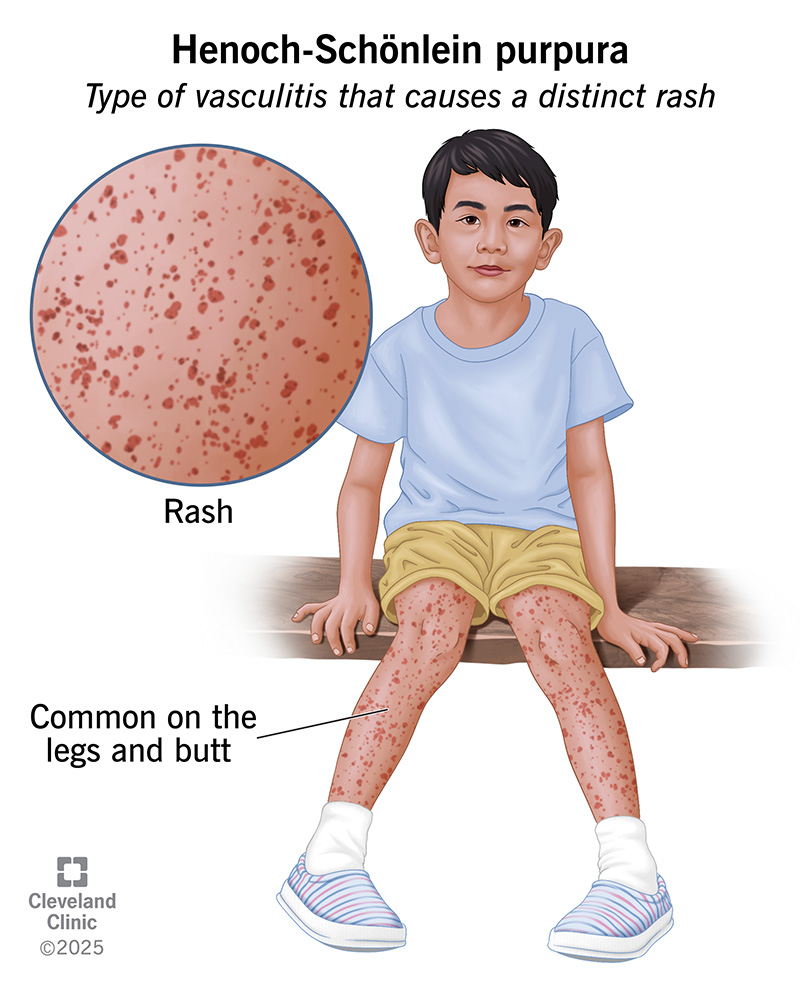
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/henoch-schonlein-purpura.jpg)
HSP symptoms can affect your child’s skin, joints, intestines and kidneys. The most common symptom is the Henoch-Schönlein purpura rash. This reddish-purple rash causes spotty, raised bumps on your child’s skin. There may be many spots or just a few. But it isn’t painful, and it usually doesn’t itch. It most commonly affects your child’s legs and butt.
Other symptoms of HSP disease may include:
Advertisement
HSP is an autoimmune disease. It occurs when your child’s immune system attacks their healthy blood vessels by mistake. Researchers don’t know why this happens. But about 50% of children have an upper respiratory infection just before the condition develops.
HSP may be an unusual reaction of your child’s immune system in response to:
IgA vasculitis can affect anyone at any age. But more than 90% of cases are diagnosed in children between the ages of 3 and 10 years old.
Other risk factors include:
Most people with HSP recover completely without treatment within three months. The condition may return but will usually go away on its own again. Sometimes IgA vasculitis can be severe and cause complications. This is even more likely in adults.
Complications of HSP disease may include:
Your child’s pediatrician will perform a physical exam. They’ll look for the telltale rash and check for joint swelling. They’ll also ask you about your child’s other symptoms and medical history. Your child’s provider may request several tests to confirm the diagnosis.
Tests to diagnose Henoch-Schönlein purpura may include:
Henoch-Schönlein purpura treatment consists of symptom relief at home. Your child may not need more than an over-the-counter (OTC) pain reliever to help with joint pain and swelling. You can try Tylenol® or an NSAID, like Advil®.
For more severe symptoms (abdominal pain, bleeding), your child’s provider may prescribe a steroid, like prednisone. If the rash and other symptoms don’t go away, see their pediatrician.
IgA vasculitis is most often a mild illness that goes away on its own. But it can cause serious complications in your child’s kidneys and intestines. Some children may need to take a medication that keeps their immune systems working correctly. It can help prevent these complications. Ask your child’s pediatrician about the side effects of these medications. That way, you can understand how they may affect your child.
Yes, most cases of HSP get better on their own without treatment. Symptoms of the condition can last up to three months. Most often, they go away after a month. While less common, symptoms may come back in the future or last longer than three months.
Advertisement
Visit your child’s provider if they experience:
No, HSP disease usually goes away within one to three months. For most children, it only occurs one time. Some children may experience a second episode. Symptoms are typically less severe the second time, and the condition often goes away on its own again.
Henoch-Schönlein purpura in children almost always has a very good outlook. Your child’s pediatrician will likely want your child to come in for follow-ups for a while to check for signs of kidney disease. While rare, long-term kidney damage can happen.
Henoch-Schönlein purpura, or IgA vasculitis, can cause your child pain and discomfort. It may be a while before they feel better again. It hurts to see your child in pain. But most children make a full recovery without any long-term complications.
Treatment isn’t always necessary. But if you’re worried or your child is uncomfortable, visit their pediatrician. You can count on their provider to listen to your concerns and help your child find relief.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your child is diagnosed with pediatric vasculitis, they’ll need expert care. And you’ll want the best team on their side. Cleveland Clinic Children’s is here for you.
