Anaplastic thyroid cancer (ATC) is a rare and very aggressive form of thyroid cancer. It grows quickly and often spreads to other areas of your body. Treatment involves surgery, radiation therapy and chemotherapy. While the outlook is often poor, some people with ATC have lived for years after treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
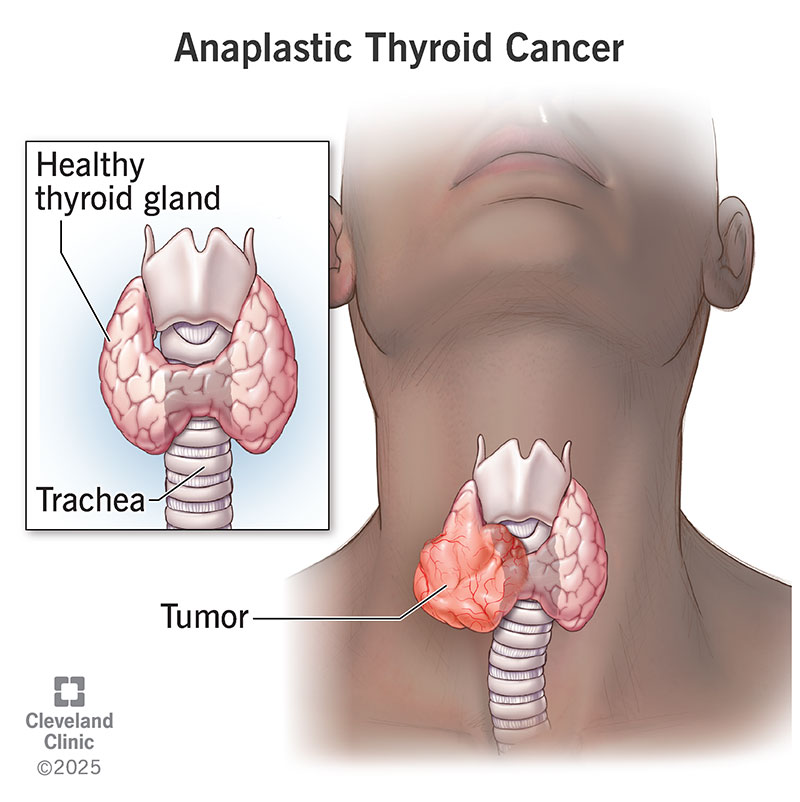
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23539-anaplastic-thyroid-cancer-atc)
Anaplastic thyroid cancer, also known as anaplastic thyroid carcinoma, is a rare and aggressive form of thyroid cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
ATC is also called undifferentiated thyroid cancer because the cells don’t look or behave like typical thyroid cells. Usually, doctors stage cancer based on the size of the tumor and if it has spread. But ATC is always stage IV. This is because the tumor is so aggressive that it has usually already spread by the time of diagnosis.
Anaplastic thyroid cancer is extremely rare. It makes up less than 2% of all thyroid cancer cases.
Anaplastic thyroid cancer most often starts as a lump or nodule on the front of your neck. You can typically see it and feel it. The lump is usually painful and hard.
If the tumor grows large enough, it can press on other structures in your neck and cause symptoms like:
People with anaplastic thyroid cancer that has spread may also have:
Scientists don’t know the exact cause. They’re trying to learn more about what may cause it.
Risk factors include:
Advertisement
Healthcare providers typically perform a needle biopsy to diagnose anaplastic thyroid cancer. During this procedure, your provider takes a small tissue sample (biopsy) from the mass on your thyroid using a very thin needle. A pathologist will look at the tissue under a microscope to see if there are cancer cells. Then, they’ll analyze what type of thyroid cancer it is.
You may need tests to see if the cancer has spread, including:
Everyone with anaplastic thyroid cancer receives a stage IV diagnosis due to the aggressive nature of this tumor. There are three substages, including:
You’ll need treatment for anaplastic thyroid cancer as soon as possible, including:
Your healthcare team will likely recommend surgery to remove the tumor unless you have other medical conditions that make surgery too risky.
Debulking surgery is the most common procedure in ATC treatment. It involves surgically removing as much of the tumor as possible. Especially any part of the tumor that’s threatening your airway.
In many cases, surgery isn’t possible. The tumor’s large size, location and invasiveness can all make it unsafe to have surgery.
Your healthcare team will likely recommend a certain type of radiation therapy called external beam radiation therapy (EBRT). This therapy directs precisely focused X-rays to areas that need treatment. Your surgeon will target the tumor itself or cancer that has spread.
Chemotherapy is a type of cancer treatment that works by destroying cancer cells and preventing them from multiplying. Your healthcare team may recommend chemotherapy as adjuvant therapy. This means that chemotherapy destroys cancer cells after surgery or radiation therapy. Chemotherapy makes radiation therapy more effective.
New chemotherapy drugs that have shown promise in treating other advanced cancers are becoming more available for advanced thyroid cancer treatment. These drugs rarely cure advanced cancers that have spread widely throughout your body. But they can slow down or partially reverse the growth of cancer.
Advertisement
Chemotherapy drugs used for thyroid cancer include:
Palliative care is medical care that relieves pain, symptoms and stress from serious illnesses. Your healthcare team may recommend palliative care to manage symptoms of ATC and the side effects of the treatment.
ATC is difficult to predict and manage due to its aggressive nature.
Having a clear view of your prognosis may be the best way to take care of yourself. Ask your healthcare provider what you can expect. These aren’t easy conversations, but they’re important. Your provider can help you understand what’s happening to your body and what might happen.
The treatment is challenging, but it’s important not to give up hope when you’re first diagnosed.
Work with a team of healthcare providers who have experience with anaplastic thyroid cancer. If you’re unable to travel to a major medical facility that has experience with it, don’t be afraid to ask your local providers to collaborate with experts on your treatment plan.
The average survival rate of anaplastic thyroid cancer (ATC) is five to six months after diagnosis. That means most people die within a few months. Fewer than 2 in 10 people with ATC live with it for more than a year.
Advertisement
Life expectancy statistics are only averages. There’s no guarantee how long you’ll live. Your healthcare providers are your best resource. They’ll help you understand what you can expect and how to plan for the future.
Due to the aggressive nature of anaplastic thyroid cancer and the lack of effective treatment options, the prognosis is often poor.
Most people who have ATC die within 12 months.
People with ATC who have the following factors generally have a better prognosis:
Hospice care helps people who have advanced, terminal illnesses. It’ll help you live comfortably.
When people are fighting a serious illness, their time and energy are often focused on their medical treatment. Hospice shifts the focus from trying to cure an illness to how you want to spend the time you have. Most people decide to enter hospice care after discussing the idea with their healthcare provider, family and other loved ones. If you’re considering hospice care, ask for help finding information and resources.
Receiving a cancer diagnosis is unsettling, regardless of the type. Given the poor prognosis of anaplastic thyroid cancer, it can be especially daunting. While treatment for ATC is challenging, it’s important not to give up hope if you receive a diagnosis. If you’re struggling with the idea of a possibly terminal illness, talk to your healthcare team. They’ll find resources to help you find your way.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Hearing you have cancer can be scary. But most thyroid cancer is treatable, and the providers at Cleveland Clinic are here to help.
