An ostomy is a surgery that creates a new opening in your body for waste to come out. Ostomy surgery bypasses either your intestinal or urinary tract and diverts it to a new opening in your abdomen. Poop or pee will now exit your stoma into a pouch (ostomy bag) that you wear on the outside of your body. An ostomy can be temporary or permanent.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
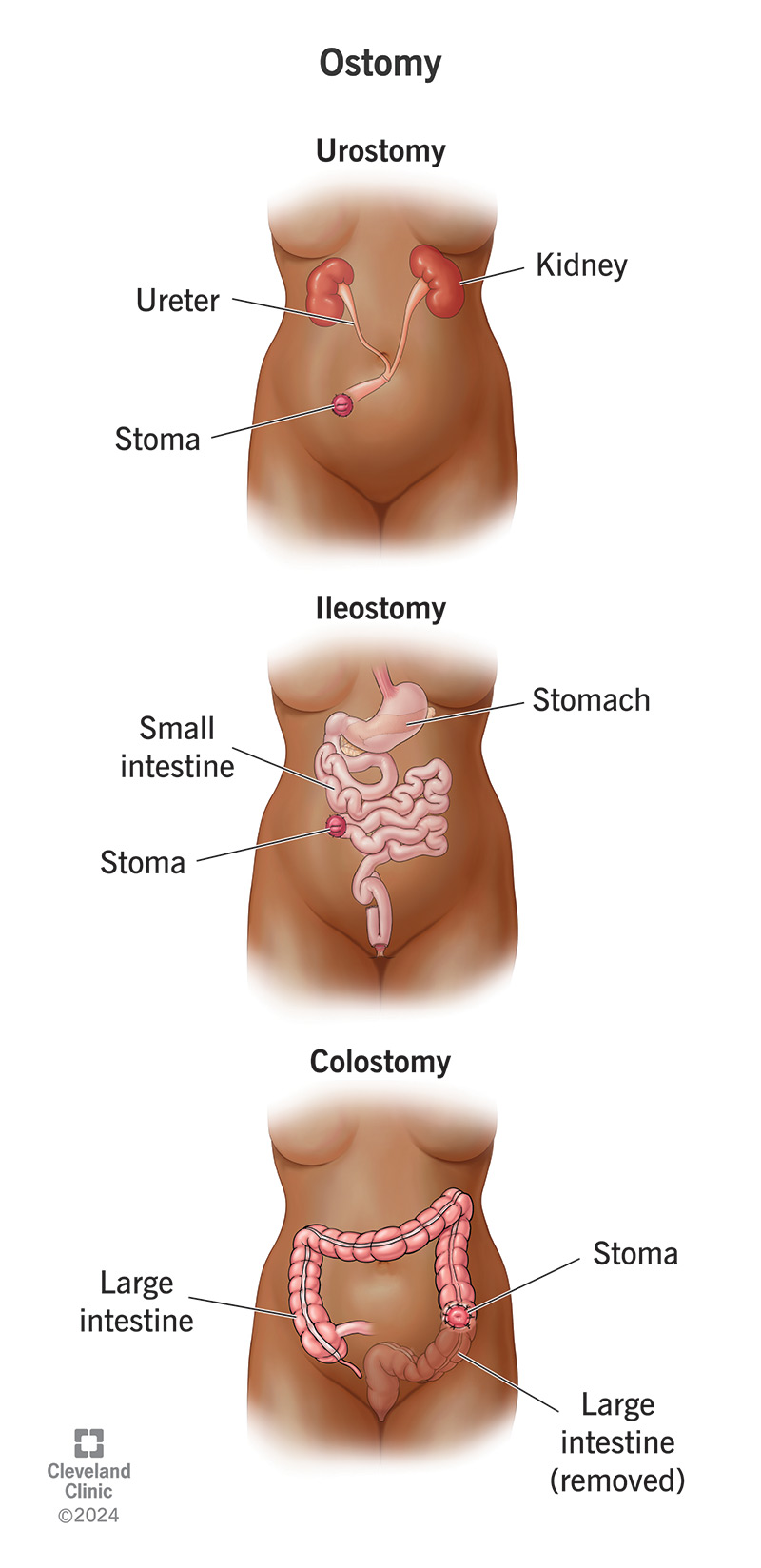
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22496-ostomy.jpg)
An ostomy is a surgical operation that helps your body remove waste (poop or pee) when the usual way of removing it isn’t working. You might need an ostomy if part of your digestive tract or urinary tract is damaged or needs time to heal.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
During ostomy surgery, a surgeon creates a small opening in your belly, called a stoma, for waste to come out. They separate the functional part of your digestive or urinary tract from the dysfunctional part and connect it to your stoma.
After an ostomy, poop or pee comes out of your stoma instead of your genitals. The waste collects into a pouch (ostomy bag) that you wear attached to your stoma. This new arrangement may be temporary or permanent.
A temporary ostomy can give your digestive or urinary tract a chance to heal after surgery or disease. A permanent ostomy can replace the damaged part of your digestive or urinary tract if it’s permanently damaged or must be removed.
You may need an ostomy if you have:
They’re more common than you might realize. About 1 in every 500 Americans lives with an ostomy.
The type of ostomy you have depends on which part of your digestive or urinary tract your surgeon is bypassing.
Advertisement
Prior to your ostomy surgery, you’ll meet with your medical team to discuss the details of the procedure. During this appointment, a healthcare provider will determine the best location for the stoma in your abdomen and mark it.
You’ll have general anesthesia for your procedure. If you have open surgery (laparotomy), your surgeon will make one long incision in your abdomen. If you have minimally invasive surgery (laparoscopic), they’ll make several small incisions.
Ostomy surgery usually occurs as part of a larger surgery. So, the steps can vary depending on the condition your surgeon is treating. Your surgeon may need to remove diseased tissue or make other repairs in your digestive or urinary tract.
When it’s time to create your ostomy, they’ll divide your digestive or urinary tract above the diseased or nonfunctioning part. They’ll create your stoma at the place marked on your abdomen and connect your bowel or ureter to this opening.
If you don’t have enough healthy intestine or ureter to connect to your stoma, your surgeon will create an extension piece to bridge the gap, or to hold more waste. They create it from a piece of your intestine. This is called an ileal conduit or ileal pouch.
You’ll spend a few days in the hospital after ostomy surgery. During this time, your healthcare team will monitor your recovery and care for you closely. You’ll also learn all about how to care for your stoma and living with an ostomy bag.
If you need to have part of your digestive system or urinary system removed, or if you need to stop using it, an ostomy can be lifesaving. It allows the functional parts of these systems to continue working without the dysfunctional parts.
In other cases, an ostomy can improve your quality of life. If you live with a chronic disease that causes you constant distress at the toilet or at other times, ostomy surgery can be a way out. It can allow you to live without these complications.
The risks and complications of ostomies can range from mild to severe. They include:
Advertisement
Your healthcare provider will explain how to recognize signs of possible ostomy complications.
It may take up to eight weeks to recover completely from ostomy surgery. Your bowel movements may take a few weeks to become regular again. Getting up and moving a little each day will help you recover faster.
After ostomy surgery, you’ll wear an ostomy bag most or all of the time. A wound ostomy continence nurse (WOCN) will show you how to attach, empty and change the pouch. Most pouches include a disposable liner and a skin barrier.
It depends on the type of pouching system you have. Most people will need to change their ostomy bags every three to seven days. Some need or prefer to change it daily. When changing your ostomy bag, be sure to:
In addition to keeping your stoma clean, be sure to examine it daily and notice any changes. If the size, shape or color looks different from normal, or it feels swollen or sore, contact your healthcare provider immediately.
If you’ve recently had ostomy surgery, it can be challenging to know which symptoms warrant a call to your healthcare provider. Trust your instincts and call if something doesn’t seem quite right. Call right away if you develop:
Advertisement
Sometimes, an ostomy is reversible. This depends on your overall health after ostomy surgery. If your digestive or urinary tract recovers and becomes fully functional again, you can discuss ostomy reversal with your surgeon at that time.
After an ostomy, you’ll still use the toilet to poop or to pee, but not for both. If you have a urostomy, you’ll still use the toilet to poop, but not to pee. If you have a colostomy or ileostomy, you’ll use the toilet to pee but not to poop.
You’ll also use the toilet to empty your ostomy bag. With an ostomy, you won’t be able to control when your pee or poop comes out and collects into your pouch. But you’ll still decide when to go to the bathroom to empty or change it.
Having an ostomy has no effect on your lifespan, and it doesn’t prevent you from living a full, active life. The condition that caused you to need an ostomy may or may not affect these things. Sometimes, an ostomy extends your life.
Ostomy surgery can save or greatly improve your life. This may be cause for relief, or even celebration. At the same time, hearing that you need an ostomy can feel scary, embarrassing or uncertain. These are all perfectly normal responses.
Advertisement
Whether it’s temporary or permanent, having an ostomy is a significant life change. Consider talking to a therapist or joining a support group as you begin this journey. Talking with others who’ve gone through it can help you learn to adjust.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Some conditions like rectal and colon cancer, Crohn’s disease and ulcerative colitis may require colorectal surgery. Cleveland Clinic has the expert care you need.
