A high-risk pregnancy is a pregnancy that involves increased health risks for you, the fetus or both. Certain health conditions and your age (being over 35 or under 17 when pregnant) can make a pregnancy high risk. These pregnancies require close monitoring to reduce the chance of complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
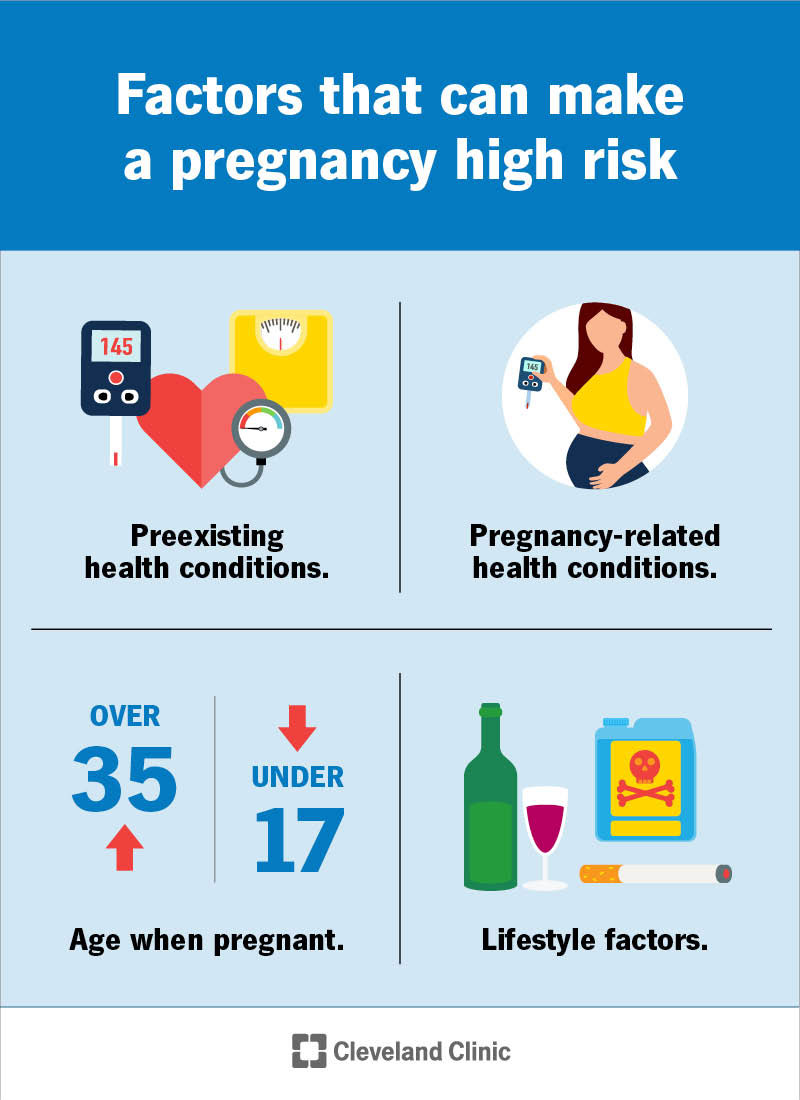
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22190-high-risk-pregnancy)
All pregnancies carry risks. The definition of a high-risk pregnancy is any pregnancy that carries increased health risks for you, the fetus or both. People with high-risk pregnancies may need extra medical care before, during and after they give birth. This helps to reduce the possibility and severity of complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
But having a pregnancy that’s considered high risk doesn’t mean you or the fetus will have health problems. Many people experience healthy pregnancies and normal labor and delivery despite having special health needs leading up to the birth.
It can be easy to panic and worry when you hear your pregnancy care provider say your pregnancy is at a higher risk. You’re not alone. It doesn’t mean your pregnancy will automatically be difficult. It may just mean your pregnancy care team watches you more closely. Trust your healthcare team’s recommendations and ask them for help managing your feelings. Many people have high-risk pregnancies, and most end in healthy babies. Routine prenatal care can help ensure your pregnancy is safe, even if it’s high risk.
Approximately 30,000 to 50,000 pregnant women (between 6% and 8%) in the U.S. have high-risk pregnancies per year.
A high-risk pregnancy means you have a higher-than-average risk of experiencing a pregnancy complication. Some pregnancies begin as high risk, while others become high risk at some point during the pregnancy.
Factors that make a pregnancy high risk include:
Advertisement
People with preexisting conditions have increased health risks during pregnancy. Some of these conditions include:
Pregnancy-related health conditions that can cause potential complications include:
These factors are only some of the conditions or factors that may result in your provider calling your pregnancy “high risk.” The label isn’t meant to scare you. Rather, it’s a way for your provider to recognize and identify potential complications to keep you and the fetus safe through pregnancy and delivery.
Talk to your pregnancy care provider right away if you experience any of the following symptoms during pregnancy, regardless of if your pregnancy is high risk or low risk:
Age alone isn’t a determining factor in a high-risk pregnancy. Your pregnancy care provider determines if your pregnancy is likely to have complications based on several other factors.
A high-risk pregnancy can be life-threatening for you or the fetus. Some of the most common complications can include:
Advertisement
It’s important to talk to your pregnancy care provider about your risks for these complications. Ask them any questions you have. With proper monitoring and care, you and your providers may be able to reduce your risk of having these or other complications.
Getting early and thorough prenatal care as soon as you know you’re pregnant is critical. It’s the best way to detect and manage a high-risk pregnancy. Be sure to tell your healthcare provider about your health history and any past pregnancies. If you do have a high-risk pregnancy, you may need special monitoring throughout your pregnancy.
Tests to monitor your health and the health of the fetus during pregnancy may include:
Management for a high-risk pregnancy will depend on your specific risk profile. Your care plan may include:
Advertisement
If there are signs that the pregnancy is in danger, your healthcare provider may recommend labor induction or a cesarean delivery earlier than planned.
It depends. Typical low-risk pregnancies have two to three ultrasounds throughout pregnancy. How many additional ultrasounds your pregnancy care provider recommends will be unique to you (but you’ll likely have more than three). Your provider will let you know how many additional ultrasounds you can expect to have if your pregnancy is high risk and when these should happen.
Many people who have high-risk pregnancies don’t experience any problems and deliver healthy babies. But they may be at a higher risk for health problems in the future, including:
Some high-risk pregnancies can increase your child’s risk of:
Advertisement
Just because your pregnancy is high risk, it doesn’t mean you or your baby will have any of these long-term medical problems. Talk to your healthcare provider to better understand your risk and your baby’s risk for these conditions.
Most people can work, go to school and continue with their typical lifestyle during a high-risk pregnancy. Discuss your work arrangements with your provider to see what they recommend and what your options are.
You can reduce your risk of pregnancy complications by:
If you’ve just learned that your pregnancy is high risk, you may be feeling anxiety, worry and many other emotions. So much of pregnancy is out of your control. Hearing your pregnancy has risk factors for potential complications can feel scary. First, try to relax and trust your healthcare team. They’re doing what’s best for you so that your pregnancy ends in a successful delivery and a healthy baby. This can feel challenging at times, but remember, they’re here to help you and to answer your questions.
Other things you can do to stay positive during a high-risk pregnancy are:
Going to all of your prenatal appointments and imaging tests is one of the best things you can do to increase your chances that a high-risk pregnancy has a successful outcome.
Contact your pregnancy care provider if you notice any of the following during pregnancy:
Pregnancy-related complications may occur up to six weeks after a pregnancy ends. Pay close attention to your health. Alert your healthcare provider right away if you notice anything abnormal after delivery.
You may hear the words “high risk” and fear that you or your baby are in danger. What does high-risk pregnancy mean? A variety of factors can make a pregnancy high risk. These include certain preexisting health conditions and new challenges that arise during the pregnancy. Try to relax until you talk to your healthcare providers and get all the information. In most cases, a high-risk pregnancy ends in a healthy baby.
Having a high-risk pregnancy means you may need special care before, during and after your baby’s birth. This can mean more prenatal ultrasounds and more careful monitoring or receiving treatment throughout pregnancy to keep you and your baby healthy. Getting thorough and frequent prenatal care is key to a successful high-risk pregnancy. Be sure to stay in close communication with your healthcare providers to reduce your risk of complications. Don’t be afraid to ask any questions you have so that you know what to expect.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Worried about your high-risk pregnancy? Want the best maternal and fetal health care? Look no further than Cleveland Clinic. We’re here for all your needs.
