Placenta previa is a condition during pregnancy where the placenta blocks all or part of your baby’s exit from your vagina. The most common symptom is vaginal bleeding in the second half of pregnancy. People with placenta previa typically need a C-section delivery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
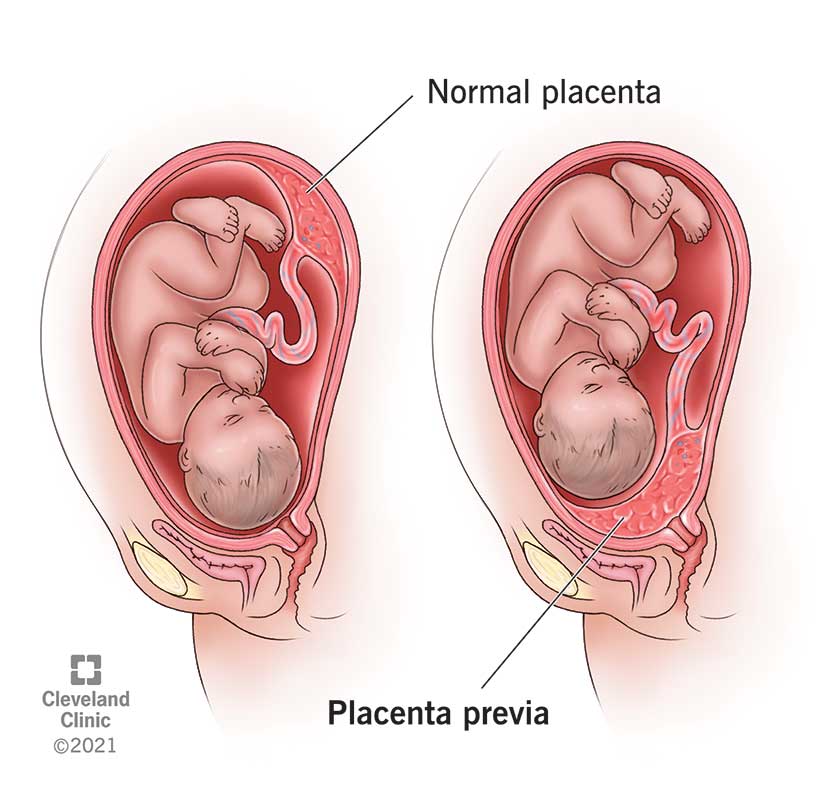
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24211-placenta-previa)
Placenta previa is a condition when the placenta blocks all or part of your cervix in the last months of pregnancy. The placenta develops in your uterus during pregnancy. It’s a sac-like organ that supplies oxygen and nutrients to the fetus through the umbilical cord.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The placenta stretches and grows through pregnancy. It’s common for it to be low in your uterus in early pregnancy. In the third trimester (weeks 28 to 40 of pregnancy), the placenta should move to the top of your uterus. This happens so your baby has a clear path to the vagina for delivery. Placenta previa occurs when the placenta doesn’t move to the top of your uterus. This means the placenta is blocking your baby’s exit from your vagina.
There are several types of placenta previa:
Each type of placenta previa can cause vaginal bleeding during pregnancy and labor. Due to the high risk of bleeding, most people will require a Caesarean (C-section) delivery.
Placenta previa occurs in about 1 in 200 pregnancies. Pregnancy care providers usually diagnose it in the second trimester during an ultrasound.
Advertisement
In placenta previa, the placenta is covering all or part of your cervix. Even though the placenta is in a complicated position, it’s still attached to your uterus. A placental abruption is when the placenta detaches from your uterus. Both conditions can cause vaginal bleeding during pregnancy and labor.
Placenta previa isn’t the same as anterior placenta. Your placenta can grow anywhere in your uterus. An anterior placement of the placenta means the placenta has implanted in the front of your body. Think of anterior placenta as a pillow between your baby and your stomach.
The most common symptoms of placenta previa are:
The amount of vaginal bleeding can vary and is often not accompanied by any pain.
There isn’t a known cause of placenta previa. There are some factors that can increase your risk of developing placenta previa, including your medical history and certain lifestyle habits.
There are several factors that increase your risk for placenta previa during pregnancy:
If you have placenta previa, there are risks for both you and your baby. Complications from placenta previa include:
For you:
For baby:
Advertisement
Yes, it’s possible to have placenta previa and not experience vaginal bleeding. You could have mild cramping or pain in your pelvic region or back. It’s best to discuss any bleeding or pelvic pain you have with your healthcare provider.
There are two main reasons you bleed if you have placenta previa. They have to do with how your body prepares for labor.
Miscarriage occurs when you experience a loss of pregnancy before 20 weeks. Pregnancy care providers don’t typically diagnose placenta previa until around or after the 20th week of pregnancy. It’s uncommon that placenta previa would be the cause of a miscarriage.
Pregnancy care providers usually identify placenta previa in a routine ultrasound around 20 weeks of pregnancy. It’s sometimes found when a person experiences symptoms of placenta previa like vaginal bleeding. Your provider will recommend ultrasounds to monitor the placement of the placenta for the remainder of your pregnancy.
Advertisement
Your healthcare provider will diagnose placenta previa using ultrasounds that show the inside of the female reproductive system:
Both types of ultrasound show the images on a monitor or screen. Your pregnancy care provider will determine how much of your cervix is covered by the placenta and recommend treatment.
The goal is to get you as close to your due date as possible. Delivering via C-section is often the safest treatment if bleeding continues. Treatment of placenta previa depends on:
If your provider finds placenta previa early in your second trimester, it can get better on its own. The position of the placenta can change as your uterus expands to accommodate the growing baby. There is often less of a chance that the placenta will move higher in your uterus if your provider diagnoses you with the condition later in pregnancy.
Advertisement
If the placenta is near or covering just part of the cervix and you’re not bleeding, your healthcare provider may recommend:
For moderate to severe cases of placenta previa or frequent bleeding, other treatments could include:
Placenta previa can go away on its own if it’s found in the second trimester. Going away on its own means the placenta shifts upwards to the top of your uterus. As your uterus expands in the third trimester, the placenta may still move. The later in the pregnancy it remains covering the cervix, the less likely it is to go away. Your healthcare provider will monitor the position of the placenta to see if the condition has resolved before delivery.
Your treatment will be unique to your condition. Most people can expect:
Maybe. Your healthcare provider will consider the amount of bleeding, the position of the placenta and the baby’s gestational age before deciding if an early delivery is necessary. Around 36 weeks of pregnancy, the best option for the health of you and your baby could be an early delivery. Other times a person reaches full term or 40 weeks of pregnancy.
If you have a marginal placenta previa (the placenta is close to your cervix, but not covering it), your healthcare provider may be able to deliver your baby vaginally. This carries a risk of bleeding and may be too dangerous. Your provider will discuss the safest way to deliver your baby.
A C-section is usually the safest delivery option if you have placenta previa. If the placenta covers even a part of your cervix, a vaginal delivery can cause severe bleeding. Your provider will typically schedule your C-section in advance, but if your bleeding is too severe at any time, you may need an emergency C-section.
It’s uncommon for placenta previa to cause birth defects. Your baby may be born premature if your healthcare provider feels it’s the safest time to deliver. Premature birth carries some complications such as low birth weight and respiratory problems.
If you’ve had placenta previa in a past pregnancy, your chances of having it again are around 2%. If you become pregnant, let your healthcare provider know so that they’re aware of your medical history.
Placenta previa doesn’t impact your chances of getting pregnant again. You’ll have a small risk of getting placenta previa again if you become pregnant.
Your healthcare provider should be able to answer your questions and prepare you for treatment of placenta previa. Here are some questions you might ask:
There is nothing you can do to prevent placenta previa and no surgical or medical procedure can correct it. There are certain risk factors for placenta previa that are within your control, like not smoking or using cocaine. Once your provider diagnoses the condition, there are ways to reduce the amount of vaginal bleeding.
Call your healthcare provider immediately if you’re bleeding, cramping or experiencing pelvic pain during your pregnancy, especially in the second half of pregnancy.
If you’re experiencing severe blood loss, you should seek emergency medical care immediately. Major blood loss carries several serious side effects to both you and your baby.
Your healthcare provider will likely advise you to limit certain activities like exercise, squatting, jumping and lifting. These activities could cause bleeding. It's best to discuss your day-to-day activities with your provider so they can suggest modifications as necessary.
Most healthcare providers will advise against having sexual intercourse if you have placenta previa. It’s best to avoid any activities that can trigger bleeding or contractions, like using tampons, douching or inserting anything into your vagina.
A note from Cleveland Clinic:
Placenta previa is a treatable condition where most people go on to deliver healthy babies. You’re likely to have a safe delivery if you follow the guidance of your pregnancy care provider. Don’t be afraid to speak up if you experience any bleeding or discomfort during your pregnancy.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Worried about your high-risk pregnancy? Want the best maternal and fetal health care? Look no further than Cleveland Clinic. We’re here for all your needs.
