Cauda equina syndrome is a medical emergency that happens when an injury or herniated disk compresses nerve roots at the bottom of your spinal cord. The cauda equina nerves communicate with your legs and bladder. It causes back pain, weakness and incontinence. Quick surgical treatment may prevent permanent complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
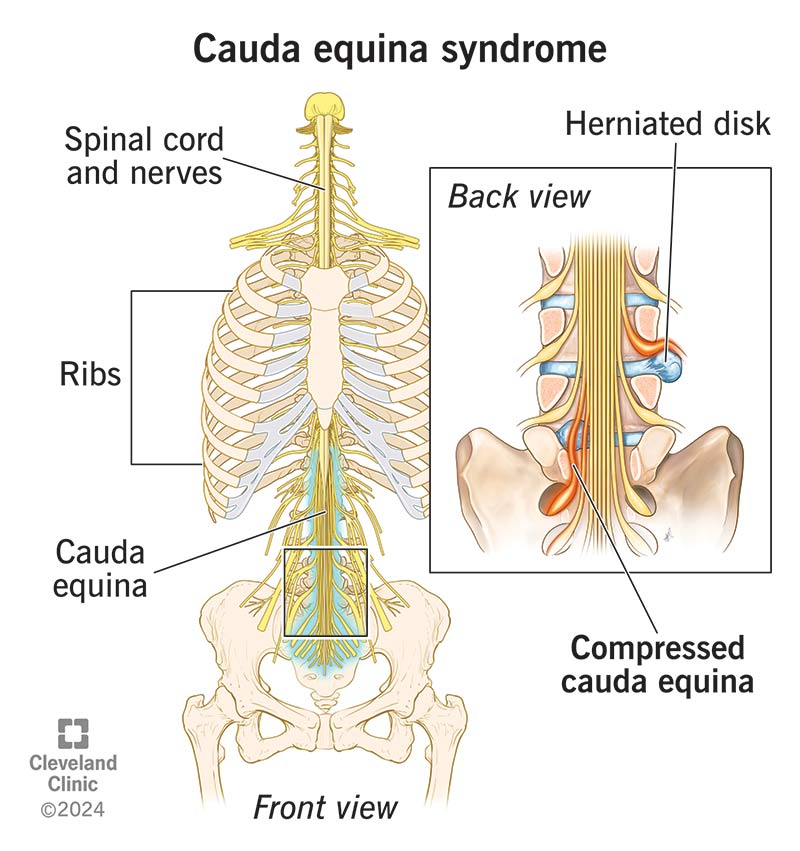
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22132-cauda-equina-syndrome)
Cauda equina syndrome is the compression of a collection of nerve roots called the cauda equina. Located at the bottom of your spinal cord, these nerve roots allow you to move and feel sensations in your legs and urinary bladder.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Nerves send and receive electrical signals all across your body. Think of nerves like power lines that send electricity to homes and businesses in your town. Severe weather may cause an old tree limb to break and fall on a power line, compressing it. This disrupts electric service to the neighborhood. First responders and electric companies are like healthcare providers and surgeons who will quickly decompress the powerlines to prevent injuries and hazards.
Compressed cauda equina nerves can cause pain, weakness, incontinence and other symptoms. Like a downed power line, if you notice symptoms, contact a healthcare provider immediately. Cauda equina syndrome can lead to permanent damage, including paralysis, if left untreated. Surgery treats cauda equina syndrome.
Cauda equina is Latin for “horse’s tail.” This collection of nerve roots is shaped like a horse’s tail.
Yes, you should seek care immediately if you notice symptoms of cauda equina syndrome. While the condition isn’t life-threatening, it can permanently damage your body, affecting your health and quality of life. Surgery might treat several of the symptoms if performed quickly.
There are two types of cauda equina syndrome:
Advertisement
Experts estimate that cauda equina syndrome affects 1 in 30,000 to 100,000 people per year around the world. It happens in an estimated 3% of all disk herniation injuries.
The symptoms of cauda equina syndrome may include:
Visit the emergency room immediately if you experience any of these symptoms.
Your ability to walk depends on what symptoms you experience. Some people don’t have any trouble walking with this condition, while others do. For example, walking may be challenging if you have weakness or numbness in your legs.
Compression — when something presses against the cauda equina nerve roots at the bottom of your spinal cord (L1 to L5) — causes cauda equina syndrome.
The most common cause of cauda equina compression is a herniated lumbar disk.
Other common causes of nerve root compression include:
If left untreated, or if there’s a delay in treatment, cauda equina syndrome may lead to nerve damage, which can cause the following permanent complications:
A healthcare provider will diagnose cauda equina syndrome after a physical exam, a neurological exam and testing. Your provider will review your medical history and assess your ability to:
This information helps your healthcare provider learn more about your:
Your healthcare provider might perform a rectal exam to check your anal muscles as well.
Advertisement
Your healthcare provider might order the following imaging tests to see your bones, nerve roots and spinal cord:
A healthcare provider may classify your cauda equina syndrome as either acute or chronic. These classifications indicate what kind of treatment you need.
Sudden cauda equina syndrome symptoms (acute) require emergency surgery. A surgeon will move whatever is compressing your nerve roots so they can heal. This surgery is called a lumbar laminectomy.
Following surgery, your provider may recommend:
Everyone heals at their own pace. You may regain feeling in your butt and legs shortly after surgery. You’ll still need to take it easy while your body heals before performing strenuous activities, even walking. It could take several weeks to months, even years before you regain control of your bladder after surgery. Your healthcare provider will explain what you can expect and what the next steps are in your healing process.
Advertisement
Cauda equina syndrome doesn’t directly affect your life expectancy. But symptoms can affect your quality of life. Seek care immediately if you notice symptoms.
Surgery can decompress your nerve roots. If treated quickly, it may prevent permanent nerve damage. Unfortunately, surgeons can’t reverse nerve damage after it happens. A healthcare provider will follow up with you after surgery to let you know how it went and what the next steps in your treatment plan look like. Regardless of your outcome, you’ll likely need long-term rehabilitation to address lingering pain, incontinence or muscle weakness.
It isn’t easy to live with a loss of bladder or bowel control, sexual dysfunction or other complications related to cauda equina syndrome. During this time, you may feel stress, depression or anxiety. You may have trouble with school, work or your relationships with friends and loved ones. Your care team will work closely with you to help you make changes to your routine and adapt. You may even choose to visit a mental health professional or join a support group to connect with others who share a similar experience.
It may not be possible to prevent all causes of cauda equina syndrome. But you might be able to reduce your risk of a herniated disk, which is the most common cause that can affect anyone. Try the following tips:
Advertisement
You should visit an emergency room immediately if you notice symptoms of cauda equina syndrome like:
Getting treatment as soon as possible reduces your risk of long-term complications.
Don’t hesitate to go to the emergency department if you experience symptoms of cauda equina syndrome. While it may feel scary, the faster you get treatment, the less likely you’ll have permanent damage to your body, including incontinence and paralysis.
It could take months to years after treatment for your body to recover. This means that you may need to manually empty your bladder and bowels. Even though it might feel embarrassing to talk to your provider about peeing and pooping, your care team is available to help you adapt and adjust your lifestyle to manage chronic symptoms.
Taking care of your mental health is just as important as your physical health with cauda equina syndrome. You may find comfort in speaking with a mental health professional or joining a support group during your recovery.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.