Thoracic endovascular aortic repair (TEVAR) is a minimally invasive procedure that treats descending thoracic aortic aneurysms. An aneurysm is a weakened area of your artery wall that bulges outward and can lead to complications without treatment. TEVAR is generally safer than open surgery and offers a faster recovery in appropriate candidates.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Thoracic endovascular aortic repair (TEVAR) is a minimally invasive procedure that repairs damage to your aorta in your chest.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your aorta is the largest artery in your body. It has many branches that supply blood to all of your organs and tissues. Many things can go wrong with your aorta, including an aneurysm (abnormal bulge in a weak area of your artery wall) or a tear in the lining of the walls (dissection). Healthcare providers commonly use TEVAR to treat aortic aneurysms and dissections in the descending thoracic aorta. Without treatment, these aneurysms and dissections can be deadly.
In years past, surgeons used open surgery to treat thoracic aortic aneurysms and dissections. But they now prefer TEVAR in many cases. That’s because TEVAR has an easier recovery and a lower risk of serious complications in appropriate candidates. Your provider will decide if you’re a candidate based on the anatomy of your blood vessels and other factors.
Surgeons use TEVAR to repair aortic damage due to:
Your healthcare provider will tell you how you should prepare. You may need to:
Advertisement
Your provider may order tests to help plan your procedure. A common test you can expect is a computed tomography (CT) angiogram. A CT angiogram can show the size and health of the arteries your provider will need to access during TEVAR.
For TEVAR to succeed, you need to have enough room in your arteries for the catheter to reach your aorta. Providers typically guide the catheter through your femoral artery (in your upper thigh) or iliac artery (in your pelvis). If these arteries are narrowed from plaque or otherwise unusable, your provider will need to find an alternative approach.
Imaging tests also help your provider choose the proper size and type of stent graft. The stent graft helps reline your artery to cover the tear in the artery in the case of a dissection or transection. For an aneurysm, the stent graft helps seal off the enlarged portion of the artery from flow to remove the risk of growing or rupturing.
Providers choose the size and type of stent graft that best suits your needs. For example, providers use a fenestrated stent graft to treat more complex aneurysms. A fenestrated stent graft has holes that allow blood to flow into arteries branching from your aorta. Such devices might be necessary for aneurysms that:
Your provider can tell you more about the type of device that’s best for you and why.
To perform TEVAR, your surgical care team will:
Advertisement
Providers sometimes use hybrid approaches for aneurysms that affect a large portion of your aorta. This means they use endovascular techniques, as well as open surgery. Your provider can tell you more about these options for aorta surgery if they’re relevant to you.
TEVAR typically takes about two hours.
In TEVAR, a catheter delivers a stent-graft to the site of your aneurysm. It serves as a new lining for your aorta.
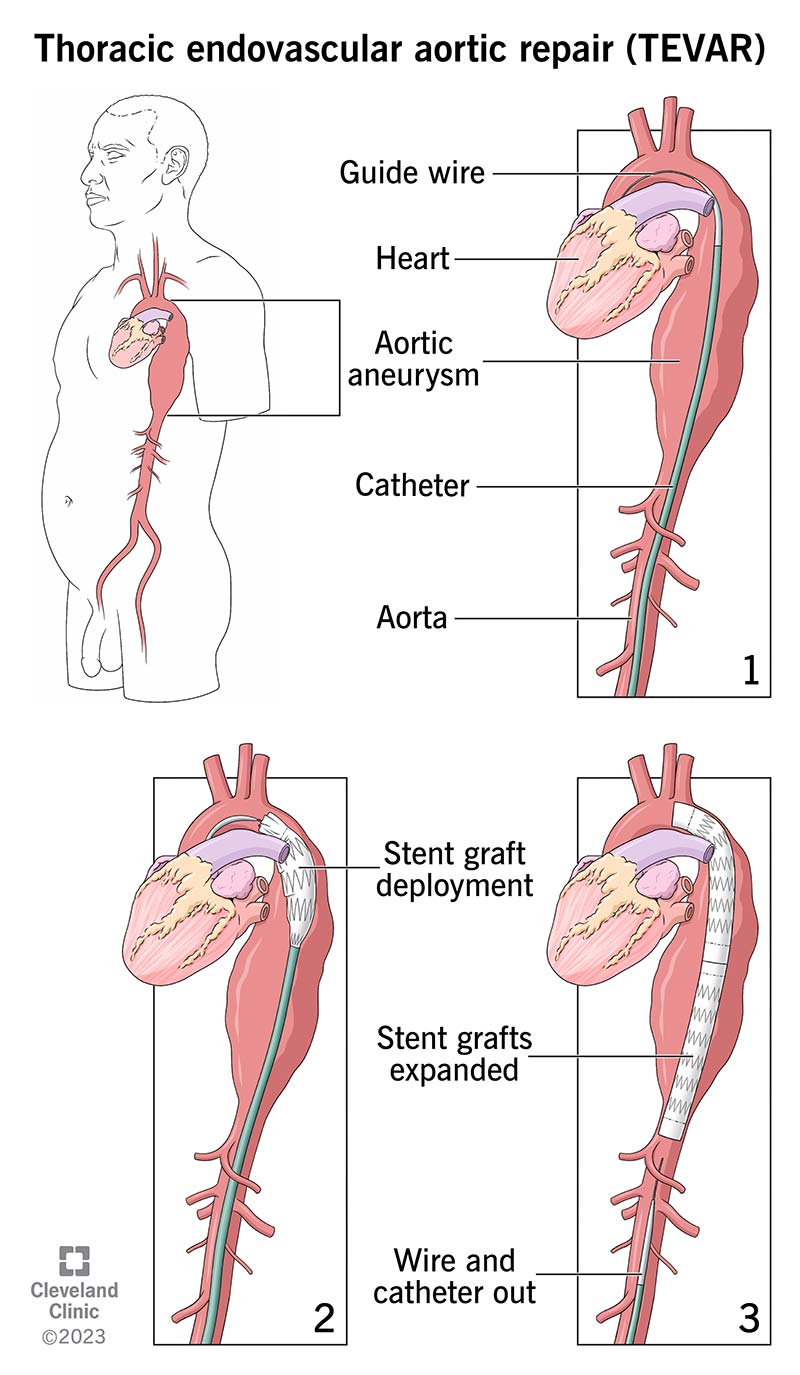
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16962-tevar-illustration)
In TEVAR, a catheter delivers a stent-graft to the site of your aneurysm. It serves as a new lining for your aorta.
You may need to stay in the intensive care unit (ICU) for one or two days after your procedure. This will depend on the area being treated. Your care team will keep a close eye on you and watch for signs of complications. You’ll then move to a regular hospital room for continued monitoring. You can expect to go home within one day to one week.
Healthcare providers typically prefer TEVAR over open surgery because TEVAR:
TEVAR has a higher survival rate than open surgery. About 98% of people survive the TEVAR procedure, while about 88% to 94% survive open surgery. Aorta centers that specialize in treating aortic disease have the best outcomes.
Advertisement
All procedures come with some level of risk. Possible risks of TEVAR include:
Talk to your provider about the risks of this procedure and what they can do to lower them.
You’ll likely go home from the hospital within a day to a week of your procedure. Follow your provider’s guidance on when you can resume normal activities. In general, you may need to:
Your provider may also recommend lifestyle changes. These include following a heart-healthy diet and getting more exercise.
Follow-ups are crucial and lifelong after any aorta surgery, including TEVAR. You can expect to see your provider for imaging tests:
The imaging tests will show if the graft is still in the proper place and if there are endoleaks or other complications. Your provider will recommend appropriate treatment if complications arise.
Advertisement
Call your provider if you have questions or concerns about your treatment plan or recovery. They’re available to answer your questions and help you feel comfortable with the process.
Call 911 or your local emergency number if you have symptoms of a heart attack or stroke. These are life-threatening medical emergencies that require immediate care.
No. TEVAR isn’t open-heart surgery. TEVAR is an endovascular procedure. That means it’s performed from the inside of your aorta using thin, long tubes called catheters and is like relining the artery from the inside.
Your surgeon makes a small incision in your skin to access one of your arteries (usually the femoral artery in your upper thigh). They use a catheter to guide a stent graft through your arteries and deliver it to the damaged area. A stent graft is a fabric tube supported by metal mesh, and it “relines” your aorta. When you have an aneurysm, placing this new lining diverts blood flow away from the weak artery walls and relieves pressure on them. This lowers your risk of complications like aneurysm rupture or aortic dissection.
Advances in technology continue to allow better treatments for people with aortic aneurysms. TEVAR is one such development, and it offers many benefits over open surgery for appropriate candidates. Your provider will determine if you’re a candidate and if the benefits of TEVAR outweigh the risks in your individual situation. They’ll also decide the best timing of treatment for you. Don’t hesitate to ask questions or share your concerns with your provider at any point along the way.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
