Video-assisted thoracic surgery (VATS) is a procedure to diagnose or treat issues in your chest. Healthcare providers often use it to diagnose or treat lung cancer. They also use VATS for esophageal cancer, lung infections and pleural effusion. Compared to open-chest surgery, VATS offers a faster, less painful recovery with fewer complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
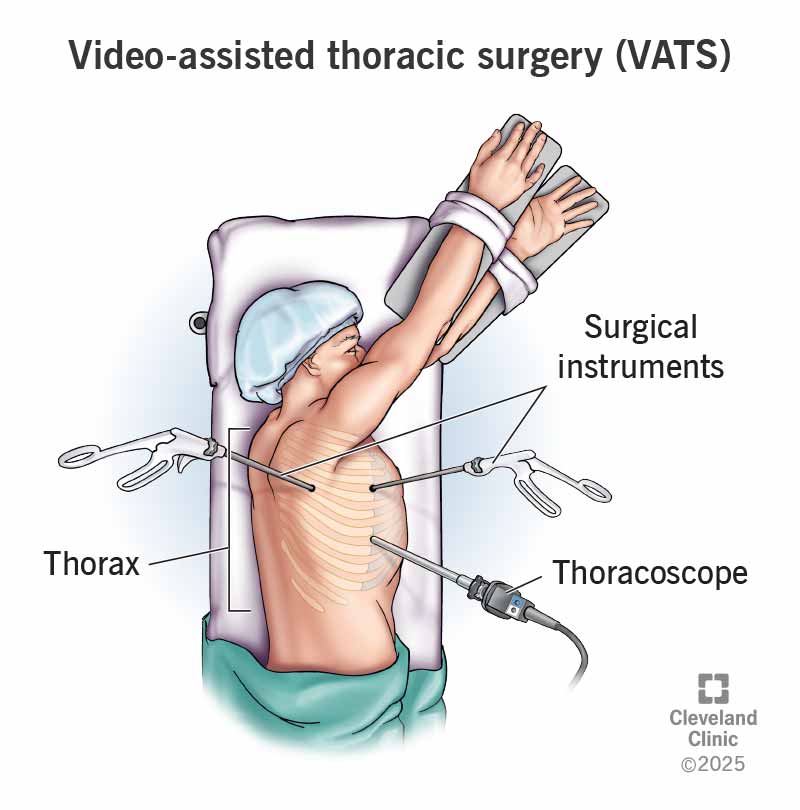
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/vats)
Video-assisted thoracic surgery (VATS) is a common procedure to diagnose and treat certain conditions that affect your chest area. Thoracic refers to the thorax, the area between your neck and abdomen that includes multiple organs. For this minimally invasive surgery, healthcare providers insert a thin tube with a tiny video camera on the end (a thoracoscope) into a small incision between the ribs in your chest. This scope allows your provider to see inside your chest cavity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your provider inserts surgical instruments into separate small incisions. They use images from the thoracoscope to guide and perform procedures. You may also hear the term video-assisted thoracoscopy.
A thoracic (chest) or cardiothoracic (heart and chest) surgeon performs video-assisted thoracoscopy. These providers have additional training in performing surgery to diagnose and treat conditions in your chest area. They’re performing VAT surgical procedures more and more often because there are many advantages for you.
Healthcare providers mostly use VATS to diagnose and treat lung cancer or metastatic cancer that spreads to your lungs.
VAT procedures also help providers diagnose and treat other thoracic conditions, like:
In a hospital or surgical center, thoracic surgeons use VAT surgery to perform different procedures like:
Advertisement
You should follow your surgeon’s instructions on what to do before the procedure. They may need you to fast (not eat or drink) for several hours before VAT surgery. Your surgeon may ask you not to take certain medications, including vitamins and herbal supplements. You may also need to quit smoking.
Before video-assisted thoracoscopic surgery, you may get tests like:
You’ll receive general anesthesia to sleep through the procedure. You’ll lie on your nonsurgical side during surgery.
Depending on the thoracic condition and VATS procedure, your surgeon will:
Some surgeons use robotic technology to perform video-assisted thoracoscopy. Your surgeon views images from the thoracoscope and operates robotic arms. They place these arms through small incisions to remove tissue or the diseased organ.
A VATS or robotic procedure usually takes two to three hours for lung cancer operations. Times for video-assisted thoracoscopic surgeries vary based on how complex the operation is.
Minimally invasive surgery often takes less time to perform than an open-chest surgery (thoracotomy). Because there’s no large incision, the recovery is less painful and often quicker.
But it’s good to remember that you have vital organs in your chest, and any procedure involves some risk.
Benefits of VAT surgeries include:
VAT surgical procedures have lower rates of complications than open procedures. But they carry a risk of complications like:
Advertisement
Your surgeon may send tissue to a lab for a biopsy. A pathologist examines the tissue for signs of cancer, infection or disease. The findings may indicate a need for additional surgery or treatments.
After surgery, your healthcare team will help you manage pain. They’ll also encourage you to do deep breathing exercises and walk around. Your healthcare provider may ask you to do physical therapy to help you recover faster and lower your chances of complications.
Before you go home, a provider will remove the chest tube they put in during VAT surgery.
Recovery time varies depending on your VATS procedure. It may take two weeks to recover from some procedures and eight weeks for others. During this time, you’ll have follow-up appointments with your provider.
Most people need to spend one or two nights in the hospital after surgery. You should carefully follow your discharge instructions. Doing so will promote a healthy recovery and lower your risk of complications.
Your at-home recovery may include:
Advertisement
Your outlook depends on the specific thoracic disorder, your overall health and the success of treatments. Your thoracic surgeon can discuss your prognosis (outlook) with you based on your diagnosis.
You should call your provider if you experience:
VATS and thoracoscopy are the same thing. Surgeons use a thoracoscope to perform thoracoscopy/VATS.
Getting a cancer diagnosis is hard enough. Any break you can get is a welcome one when it comes to treatment. Video-assisted thoracic surgery (VATS) offers a faster recovery and less pain than open-chest surgery. Your provider can tell you if this is the right procedure for you. Don’t hesitate to ask any questions you have about the procedure.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have lung cancer, you might feel alone and afraid. You don’t have to be. Cleveland Clinic is here to help find and treat your cancer at any stage.
