Atelectasis happens when lung sacs (alveoli) can’t inflate properly, which means blood, tissues and organs may not get oxygen. It can be caused by pressure outside of your lung, a blockage, low airflow or scarring. The most common cause of atelectasis is surgery with anesthesia. Atelectasis usually resolves after treating the underlying cause.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
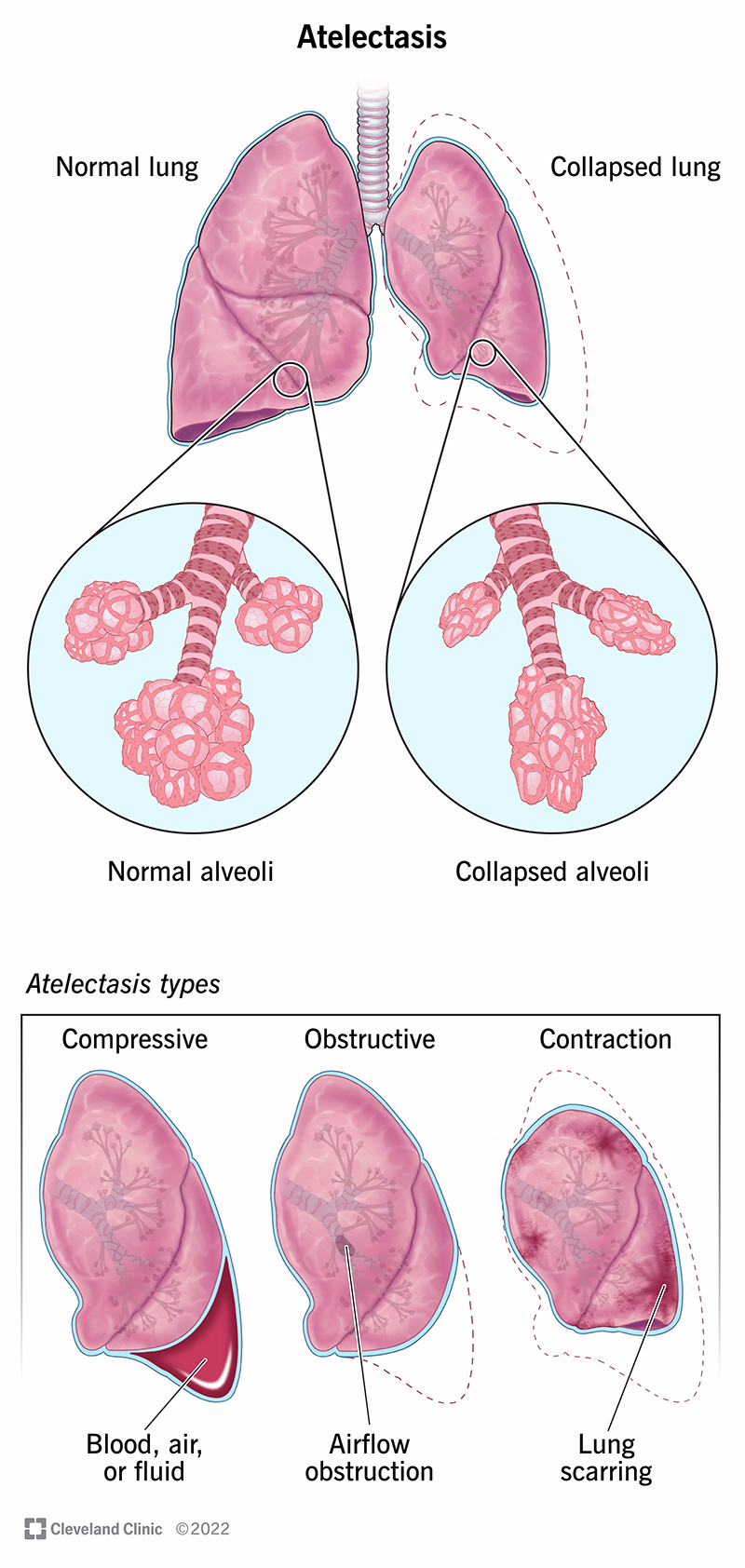
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17699-atelectasis)
Atelectasis (pronounced at-uh-LEK-tuh-sis) is the collapse of one or more parts of the lung. It specifically affects the small air sacs called alveoli.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When you breathe in, your lungs fill up with air. The air travels to sacs in your lungs (alveoli), where the oxygen moves into your blood. The blood delivers the oxygen to organs and tissues throughout your body.
If you don’t have enough air coming in to inflate your alveoli or if outside pressure is pushing on them, they can collapse (atelectasis). Atelectasis can happen in a small area or the whole lung. If enough of your lung is affected, your blood may not receive enough oxygen, which can cause health issues.
Atelectasis is a condition where alveoli in your lung or a part of your lung deflates, causing a partial or complete collapsed lung. Pneumothorax is a condition where air leaks into the space around your lung, compressing it and causing it to collapse.
If you haven’t had a chest or abdominal surgery recently, atelectasis can indicate an obstruction of your airway that’s causing a partial or complete collapse of your lung.
You’re at a higher risk for atelectasis if you have:
Advertisement
There are three main types of atelectasis: compressive, resorptive (obstructive) and contraction.
Compressive atelectasis is when something around your lung — like fluid, air, blood or a tumor — pushes against it, causing it to collapse.
Resorptive atelectasis happens when the oxygen and carbon dioxide in your alveoli move into your bloodstream and no new air moves in. This causes your alveoli to collapse. Surgery that requires anesthesia is a common cause of resorptive atelectasis.
Something blocking the inside of your lung, keeping air from coming into the alveoli, can also cause resorptive atelectasis. Also called obstructive atelectasis, the blockage can be mucus, a tumor or an object that you accidentally inhaled.
Lung scarring (fibrosis) causes contraction atelectasis. Scarring keeps the alveoli from opening properly.
Newborns, particularly premature newborns, or people with acute respiratory distress syndrome (ARDS) can have an uncommon type of atelectasis called patchy atelectasis. Patchy atelectasis happens when you don’t have enough of a protein in your lungs that helps keep them from collapsing (surfactant).
Other types of atelectasis (bibasilar atelectasis, rounded atelectasis, gravity-dependent atelectasis and subsegmental atelectasis) describe the location, appearance or severity of the collapse.
Atelectasis often causes no symptoms on its own, though some underlying conditions that lead to atelectasis (like COPD) can cause symptoms.
If atelectasis affects large areas of the lungs, the oxygen level in your blood may go down (hypoxemia). This can lead to symptoms like:
Surgery is the most common cause of atelectasis. When anesthesia is used during surgery to keep you asleep, you don’t breathe deeply enough to fill your lungs all the way or cough to clear your lungs of mucus. This can lead to blockages or lack of air to the alveoli, causing resorptive atelectasis.
Other causes of atelectasis include:
Advertisement
Chest X-rays (pictures of your lungs) are the first step in diagnosing atelectasis. Your healthcare provider may use a computed tomography (CT) scan to get more detailed pictures if necessary.
In some cases, your provider may look at the inside of your lungs using a small camera attached to a tube that goes down your throat (bronchoscopy). Blockages may be removed during bronchoscopy.
Many cases of atelectasis get better without treatment, under careful monitoring by your healthcare provider.
Other treatments depend on the cause and extent of the collapse. Treatments could include:
While atelectasis is usually not serious itself, some cases can have serious complications:
Advertisement
Most of the time, atelectasis is reversible once the cause is treated. Most people recover quickly and have no serious lasting effects. In people who have a long-lasting (chronic) condition, further treatment may be needed to manage the underlying cause of atelectasis.
Here are some ways to reduce the risk of atelectasis:
The best way to take care of yourself is to follow your healthcare provider’s recommendations for care after surgery. Make sure you manage any underlying conditions that can increase your risk of atelectasis.
If you’ve recently had surgery or have an underlying condition and have any new or worrisome symptoms, contact your healthcare provider immediately.
Your lungs are a complicated and important organ. They need to get airflow in and oxygen to your blood so that your tissues and organs work properly. Atelectasis is something that can happen when one part of that system isn’t working quite as planned. Fortunately, while “collapsed lung” — even just a partial one — sounds scary, in most cases, atelectasis isn’t a life-threatening condition.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
