A pacemaker is a small device a healthcare provider can place in your upper body, usually during a surgery, to send impulses to your heart. The electronic device can manage abnormal heart rhythms. There are several kinds of pacemakers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
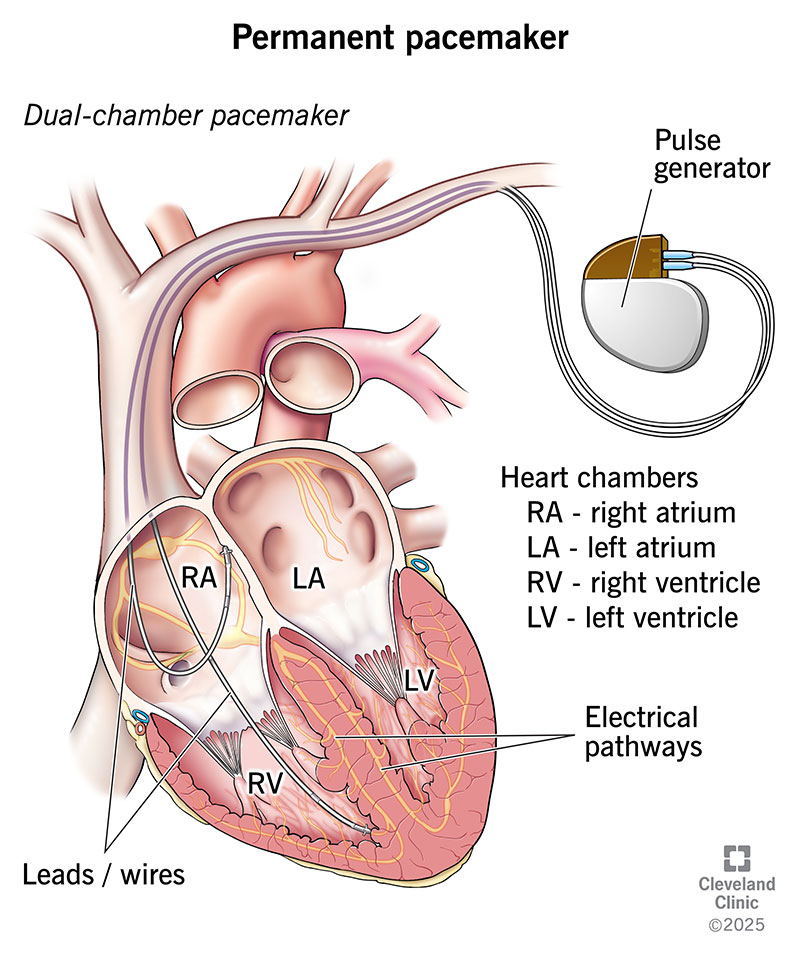
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17360-permanent-pacemaker)
A pacemaker is a device a healthcare provider places in your upper body to help your heart beat at a typical rate and rhythm. The device can stabilize abnormal heart rhythms and prevent problems that could disrupt or endanger your life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pacemakers use electrical impulses to correct problems with your heart’s electrical system. Typically, this system tells your heart’s chambers when it’s their turn to squeeze. When your heart’s electrical system doesn’t work right, your heart’s chambers may squeeze in the wrong order or too weakly. When this happens, they can’t provide enough blood to your body.
A cardiac pacemaker can sense when your heartbeat is too slow. Then, it delivers electrical impulses to control the rhythm of your heart. The device can sometimes help people with a fast or irregular heartbeat. But it can’t deliver a shock to correct the rhythm.
Talking to your healthcare provider about your concerns or symptoms is the first step to finding out if a pacemaker can help you. Pacemakers are common. They can treat problems with your heart’s electrical system, like certain arrhythmias (abnormal heart rhythms) or heart blocks. They also treat heart failure and heart palpitations (pounding in your chest). People may also need them if they’re short of breath or have unexplained dizziness or lightheadedness, nausea, confusion or fainting.
Depending on the heart problem, your healthcare provider may suggest a specific type of cardiac pacemaker with one to three wires (called leads). Types of pacemakers include:
Advertisement
Before your operation, you can expect to:
Depending on the type of cardiac pacemaker, you’ll have a catheter-based, vein-based or surgical-based operation. Approaches include:
If the pacemaker has one or more leads, your provider will attach them to the pacemaker device. Then, they’ll place the device into a small “pocket” they make from tissue under the skin in your upper chest or abdomen. After testing the device, your provider will close the cut they made for the pocket.
Catheter-based procedures usually take about an hour or less. The transvenous and surgical-based approaches take between two and five hours. Your healthcare provider will explain which is best for you. The goal is to help you feel less pain, recover faster and get back to your life sooner.
Pacemakers can improve your quality of life and prevent disruptions from heart problems. Benefits include:
Pacemaker procedures tend to have few complications, but the following are possible:
Advertisement
You might need to spend one night at the hospital, or you may go home after only a few hours. You may have an X-ray to make sure the device and wires are staying put. And your healthcare team will check your device to be sure it’s working right.
Before you go home, you’ll get a card to carry with details about your device. You’ll receive information about what can interfere with your pacemaker. For example, you should avoid spending much time near a metal detector or a store’s theft detector. Also, keep cell phones and headphones 6 inches away from your pacemaker. Some medical tests (like MRIs) and treatments may also cause issues with pacemakers.
You can most likely get back to your normal routine a few days after pacemaker surgery. It can take several weeks to fully recover after a pacemaker procedure. During that time:
You can shower four or five days after you get your pacemaker.
Your healthcare provider will schedule follow-up visits once or twice a year to check your pacemaker’s battery level. Replacing the battery is usually a simpler process than implanting the device. Pacemaker batteries can last 10 to 15 years.
Advertisement
Follow-up visits also let your provider see how you’re doing and how well your pacemaker is working.
The life expectancy of a person who has a pacemaker depends on several factors. Your age and medical conditions when you receive it are two of these factors. People who have fewer or less severe health concerns tend to live longer and are more likely to have a normal or near-normal life expectancy.
If you have a pacemaker, it’s best to manage your health and be aware of how you feel. Your healthcare provider may prescribe medicines that are meant to work along with your pacemaker. Be sure you understand how you’re supposed to take your medications and for how long.
If you have questions, be sure to ask them. Your provider is there to make sure you have the best possible outcome, and they know that’s more likely when you have the answers to all your questions.
Call your healthcare provider if you:
Advertisement
Heart problems that lead to the need for a pacemaker can make you feel stressed, anxious or scared. Your healthcare provider can help you understand your situation and talk you through it so you can feel better about what’s happening. They can help you decide which pacemaker is best for you. They can also recommend resources that can help you cope with any questions or concerns you might have.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
