Many conditions, including plantar fasciitis and Achilles tendinitis, cause heel pain. A sore heel is a common foot and ankle issue. Rest, orthotics and stretching ease pain over time. If you ignore and don’t treat heel pain, you may develop chronic problems that require a longer recovery. Heel pain rarely needs surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
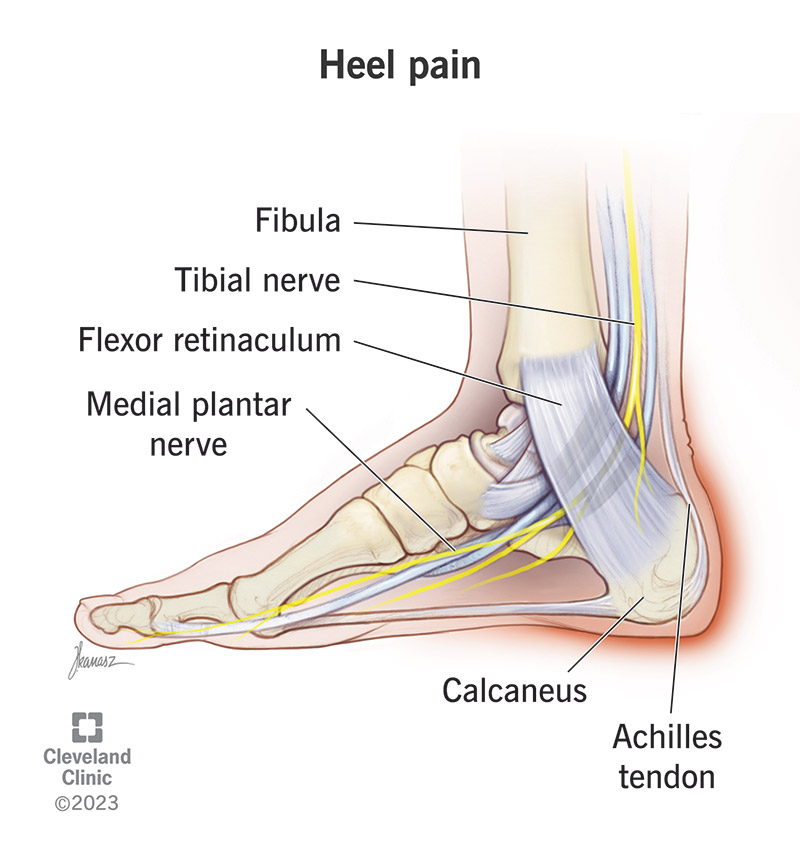
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/heel-pain)
Heel pain is a very common foot and ankle problem. You might experience pain, soreness or tenderness anywhere in your heel, but the most common areas are underneath it or the back of it. There are many different health conditions that can cause heel pain, including plantar fasciitis and Achilles tendinitis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Heel pain can make it difficult to walk and participate in daily activities. It’s important to see your healthcare provider to help you determine the exact cause of pain in the heel of your foot. Most heel conditions improve with nonsurgical treatments, but your body will need time to recover.
Heel pain causes range from mild to severe, depending on the location of the pain. You may experience sudden heel pain without injury or pain that develops over time. Several problems are located at the back of the heel:
Advertisement
Problems that cause bottom-of-heel pain include:
Anything that puts a lot of pressure and strain on your foot can cause heel pain. The way you walk (foot mechanics) and your foot’s shape (foot structure) are also factors.
You may be more likely to develop heel pain if you:
Your healthcare provider will assess your symptoms and perform a physical exam. You may also get X-rays to check for arthritis, bone fractures, bone misalignment and joint damage.
Rarely will you initially need an MRI (magnetic resonance imaging) or ultrasound. These can show soft tissue problems that X-rays don’t reveal.
Most problems that cause heel pain get better over time with nonsurgical treatments. Heel pain treatment focuses on easing pain and inflammation, improving foot flexibility and minimizing stress and strain on your heel. These treatments include:
Advertisement
It’s rare to need surgery to treat most causes of heel pain.
Heel pain can interfere with your ability to get around, work, exercise and complete daily tasks. When it hurts to move, you can become inactive (sedentary), which can lead to weight gain. You may also develop depression because you can’t do the things you love.
Untreated Achilles tendonitis can cause the tendon to break down (tendinosis). In time, your Achilles tendon can tear or rupture. This problem may require surgery.
To prevent heel pain or keep pain from returning, it’s important to keep your foot and heel tendons flexible. You should stretch regularly and wear properly fitted, supportive shoes. Runners are especially prone to heel pain. You can prevent running injuries by covering fewer miles and running on softer surfaces.
You should call your healthcare provider if you experience:
You may want to ask your healthcare provider:
Advertisement
Heel pain often improves over time with nonsurgical treatments. Your healthcare provider can determine what’s causing the pain. Your provider can also show you stretching exercises and recommend orthotics and other methods if needed. Many people try to ignore heel pain and continue with activities that make the problem worse. But it’s essential to give your body time to recover. Otherwise, you may develop chronic heel pain that sidelines you for an extended time. The longer you have heel pain, the harder it is to treat effectively, so it’s important to get evaluated.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
An aching foot or heel can bring your favorite activities to a halt. Cleveland Clinic’s foot pain experts are here to help you heal and get back on your feet.
