There are more than 30 joints in your feet and ankles, and arthritis can affect any of them. Natural wear and tear, health conditions and injuries can cause it. A healthcare provider will suggest ways to manage symptoms like pain, stiffness or reduced range of motion.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
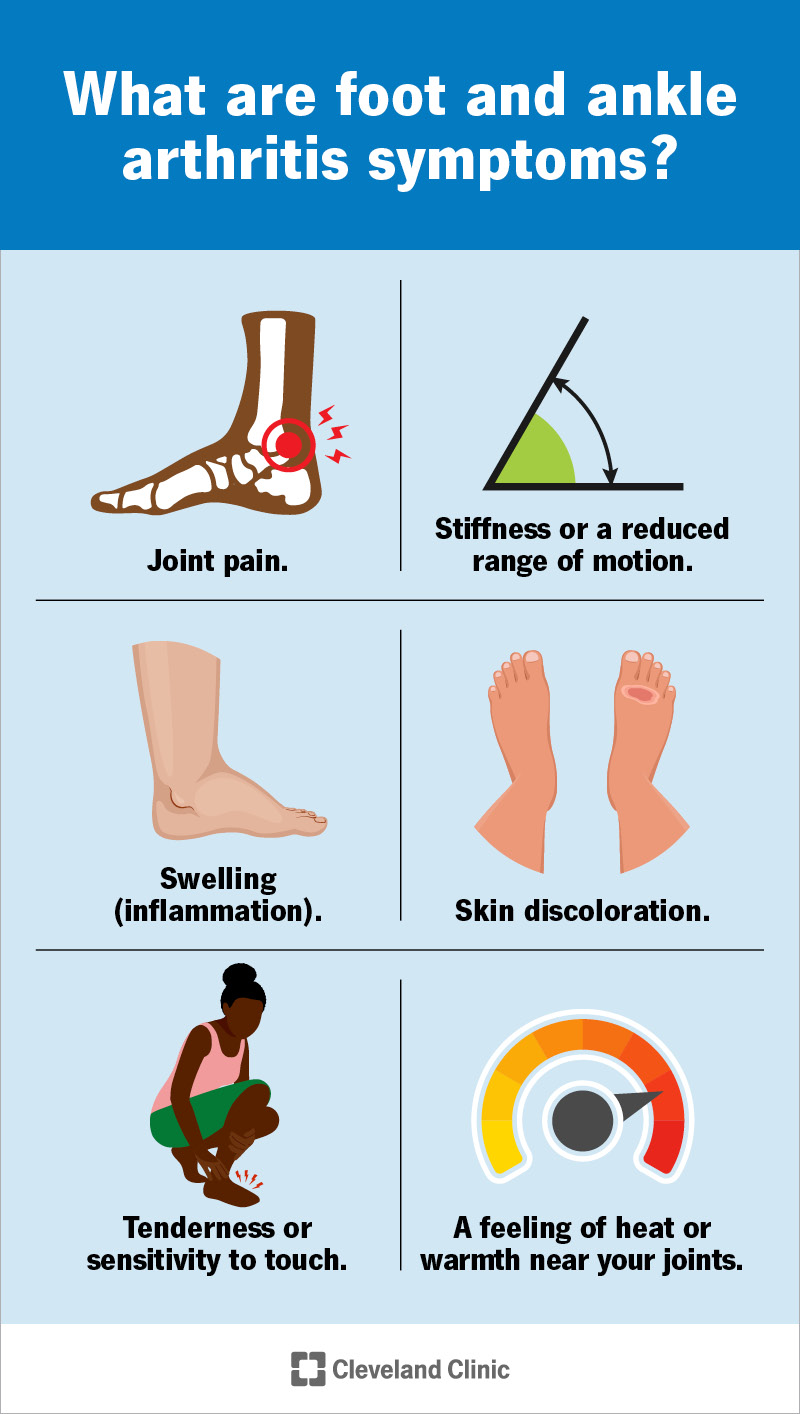
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/foot-and-ankle-arthritis-infographic.jpg)
Foot and ankle arthritis is any type of arthritis that affects joints in your feet and ankles.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These joints naturally wear down as you age. Lots of people develop arthritis after normal, lifelong wear and tear. Some health conditions and injuries can also cause arthritis in your feet and ankles.
Each of your feet has 26 bones and more than 30 joints. Arthritis can affect any of them, including your toes.
Your ankle joints are where your lower legs meet your feet. It’s common for arthritis to develop where any of the bones in your ankle meet.
Visit a healthcare provider if you’re experiencing foot pain or ankle pain that’s severe enough to affect your day-to-day routine, or if you feel like you can’t move or use your feet and ankles as well as usual.
There are more than 100 different types of arthritis. Some of the most common types that involve feet and ankles include:
The most common foot and ankle arthritis symptoms include:
Arthritis usually develops slowly over time, so you won’t suddenly know you have it. You might start noticing you’re feeling the same kind of pain or other symptoms in the same spot in your foot or ankle.
Advertisement
It might be hard to move or walk if you have arthritis in your feet and ankles. Stiffness might get better once you start moving. It’s usually worse first thing in the morning or if you’ve been sitting or lying down for a long time.
Some types of arthritis cause symptoms in waves that come and go, called flares or flare-ups. Others make your joints feel painful or stiff all the time, or after being physically active.
Where you notice signs of arthritis depends on which type you have, and which joints it affects. It’s possible to have arthritis in any section of your foot, including your:
What causes arthritis in your feet or ankles depends on which type you have:
Anyone can develop arthritis in their feet or ankles, but some factors may make you more likely to, including:
Some people have a higher arthritis risk, including:
A healthcare provider will diagnose arthritis in your feet and ankles with a physical exam. You might need to see a podiatrist. They’ll examine your feet, ankles and toes and ask about your symptoms. Tell your provider when you first noticed symptoms like pain and stiffness, and if any activities or times of day make them worse. Tell your provider if you feel symptoms in one or both feet.
Advertisement
Your provider may ask you which type of shoes you wear most often, and if any kinds of shoes make your symptoms worse. They may watch how you walk or move (a gait analysis).
Your provider will probably check your range of motion (how far you can move a joint). They may compare one joint’s range of motion to other, unaffected joints in your other foot or ankle.
Your provider might use imaging tests to take pictures of your joints, including:
Your provider may use blood tests to check your uric acid levels if they think you have gout. Blood tests can also show signs of infections or autoimmune diseases.
Which treatments you’ll need depends on what’s causing the arthritis, which type you have and which joints in your feet and ankles it affects.
The most common arthritis treatments include:
Advertisement
There’s no cure for arthritis, but your healthcare provider will help you find treatments that reduce how much (and how often) arthritis impacts your daily routine.
Some people with arthritis experience more severe symptoms as they age. Ask your provider how often you should have follow-up visits to check for changes in your feet or ankles.
Staying active is one of the best ways to relieve arthritis symptoms. Don’t force yourself to do anything that causes severe pain, but moving your body can reduce pain and stiffness and prevent symptoms from getting worse.
You don’t need to become an ultramarathoner or Olympic weightlifter. Walking, swimming, riding a bike, stretching or doing yoga are all great ways to support joints in your feet and ankles (and your whole body).
Talk to your provider about exercises that are good for you. They’ll suggest options that help you safely stay active.
Some types of arthritis happen naturally or because of health conditions you can’t control, so there’s not always a way to prevent it. However, you can lower your chances of developing arthritis by:
Advertisement
Visit your healthcare provider if you experience any of the following symptoms:
You may want to ask your provider:
Your feet and ankles carry you through your daily routine. No matter what’s causing it, arthritis symptoms like pain, stiffness and reduced mobility are frustrating at best. At their worst, they can affect how much you enjoy your favorite activities.
Don’t ignore pain or other symptoms in your feet and ankles. The occasional ache or pain is normal (especially after a long day or intense workout), but you shouldn’t constantly feel uncomfortable. Visit a healthcare provider as soon as you notice new or worsening symptoms that don’t get better on their own.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
