Haglund’s deformity is sometimes called a “pump bump” because it’s especially painful to wear shoes like pumps (high heels) that have tight backs. Once you learn to manage your symptoms and make any changes to your daily routine to avoid pain, Haglund’s deformity shouldn’t have an impact on your health.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
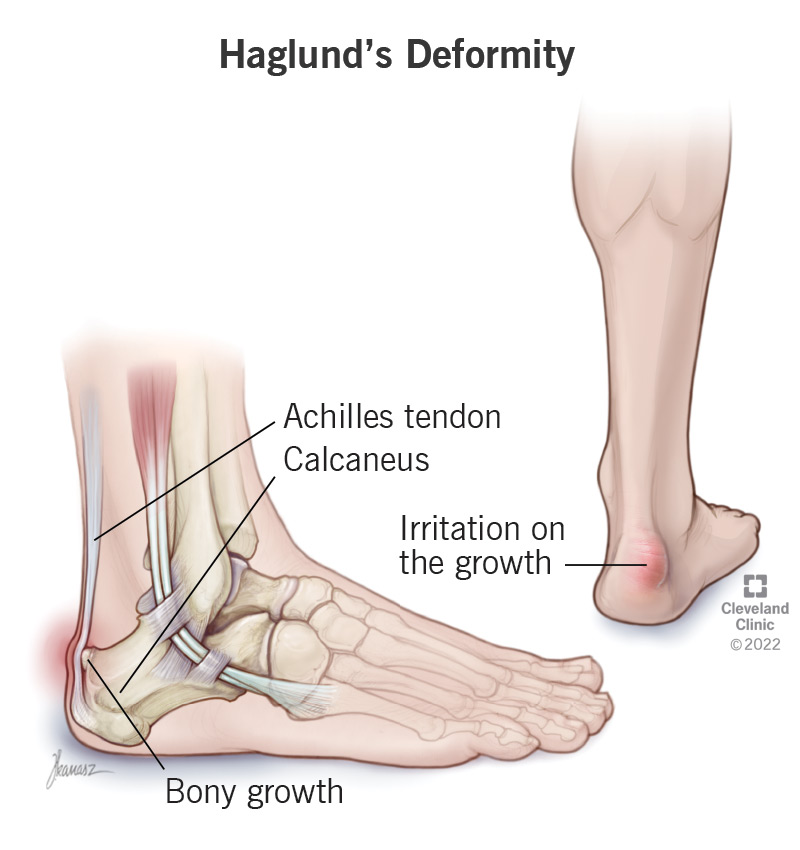
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/25134-haglunds-deformity)
Haglund’s deformity is a bony growth on your heel bone (calcaneus) where your Achilles tendon attaches. The growth causes a bump you can see and feel through your skin.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Haglund’s deformity can cause heel pain, especially when you wear shoes that press tightly against the back of your heel. Over time, pressure and irritation on the growth can cause other conditions in your heel and feet, including Achilles tendinitis and heel bursitis.
It’s usually treated with heel cups, orthotic inserts, changing the shoes you wear and over-the-counter medicines to alleviate pain.
It’s rare to need surgery to remove the growth caused by Haglund’s deformity, but some people need it if other treatments don’t relieve pain and other symptoms.
Haglund’s deformity is very common, but it’s hard for experts to estimate exactly how many people have it at any one time. Many people with mild (or no) symptoms never get their heel pain diagnosed as Haglund’s deformity.
Symptoms of Haglund’s deformity include:
Haglund’s deformity almost always develops on both feet (bilaterally).
Experts don’t know for certain what causes Haglund’s deformity. Studies have found that it might be genetically inherited (passed down through generations of a biological family).
Other causes might include:
Advertisement
Haglund’s deformity can affect anyone, but certain groups of people are more likely to develop it:
A healthcare provider will diagnose Haglund’s deformity with a physical exam and imaging tests. They’ll discuss your symptoms and feel the bump on your heel.
You might need X-rays to take a full picture of the bony growth and to see if anything else is causing issues with your foot or ankle. Your provider might use magnetic resonance imaging (MRI) before surgery (if you need it).
Your provider will suggest treatments for Haglund’s deformity that relieve your symptoms rather than removing the growth. You might need some or all of the following:
If these conservative treatments eliminate your symptoms, that’s probably all the treatment you’ll need.
It’s rare to need surgery to treat Haglund’s deformity.
Your provider will likely only recommend surgery if you have severe symptoms that haven’t gotten better after other treatments.
Your surgeon will remove the bony growth and any inflamed tissue in your heel. Most people need a few months to recover fully from Haglund’s deformity surgery
The most important way to manage your symptoms is to avoid the types of shoes or activities that make your symptoms worse.
Haglund’s deformity is sometimes called a “pump bump” because it’s especially painful to wear shoes like pumps (high heels) that have tight backs. If you know which kinds of shoes cause your pain, you should avoid them as often as possible. Some people are never able to wear certain styles of shoes, even after their symptoms get better or they have surgery to remove the bony growth.
If your provider or physical therapist gives you exercises or stretches to improve your flexibility, try to do them as often as they suggest.
Most people feel better over time as they manage their symptoms and avoid the shoes or overuse that caused their pain.
Advertisement
If you need surgery to remove the Haglund’s deformity growth, you should feel better gradually as you heal and regain your strength and ability to walk like you usually can. This typically takes between several weeks and a few months.
If you have Haglund’s deformity, you shouldn’t have any long-term issues. Once you learn to manage your symptoms and make any changes to your daily routine to avoid pain, Haglund’s deformity shouldn’t have an impact on your health.
If you don’t have the bony growth surgically removed, Haglund’s deformity is technically a lifelong condition. But once you know how to manage your symptoms (like occasional pain or swelling), Haglund’s deformity won’t impact your life or health.
You shouldn’t need to miss work or school even while you’re treating Haglund’s deformity.
If you have surgery to remove the bony growth, you might need to avoid certain activities while you’re recovering. Talk to your provider or surgeon about your specific recovery timeline and before you resume any physical activities after surgery.
Because experts aren’t sure what causes Haglund’s deformity, there might never be a way to fully prevent it from developing. It’s what’s known as an idiopathic condition, which means it can appear with no cause or trigger.
Advertisement
Even if you might not be able to totally prevent Haglund’s deformity, maintaining good foot and ankle health can help prevent pain and other issues:
Talk to your provider if you notice any of the following:
Go to the emergency room if you suddenly lose the ability to use or move your foot, or if you’re experiencing severe pain.
If you experience a trauma or think you have a bone fracture, go to the ER right away.
Advertisement
Both Haglund’s deformity and heel spurs are bony growths on your heel.
Heel spurs poke out from the bottom of your heel, where your heel bone connects to the ligament running between your heel and the ball of your foot (the plantar fascia).
Haglund’s deformity always forms at the back of your heel bone, where your Achilles tendon attaches.
Fortunately, treatment for Haglund’s deformity and heel spurs is very similar. No matter what’s causing your heel pain, talk to a healthcare provider.
Haglund’s deformity — a bony growth on your heel bone where your Achilles tendon attaches — is a manageable condition that you might never even notice you have. Even if your pain is minor — or it comes and goes — talk to your provider about any new symptoms. You might need something as simple as a new pair of shoes to feel a lot better.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
An aching foot or heel can bring your favorite activities to a halt. Cleveland Clinic’s foot pain experts are here to help you heal and get back on your feet.
