Spinal tumors can form anywhere in and along your spinal column, which includes your vertebrae, spinal cord and the tissues surrounding your spinal cord. Most spinal tumors result from cancer metastasis — cancer that has spread from another area of your body to your spine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
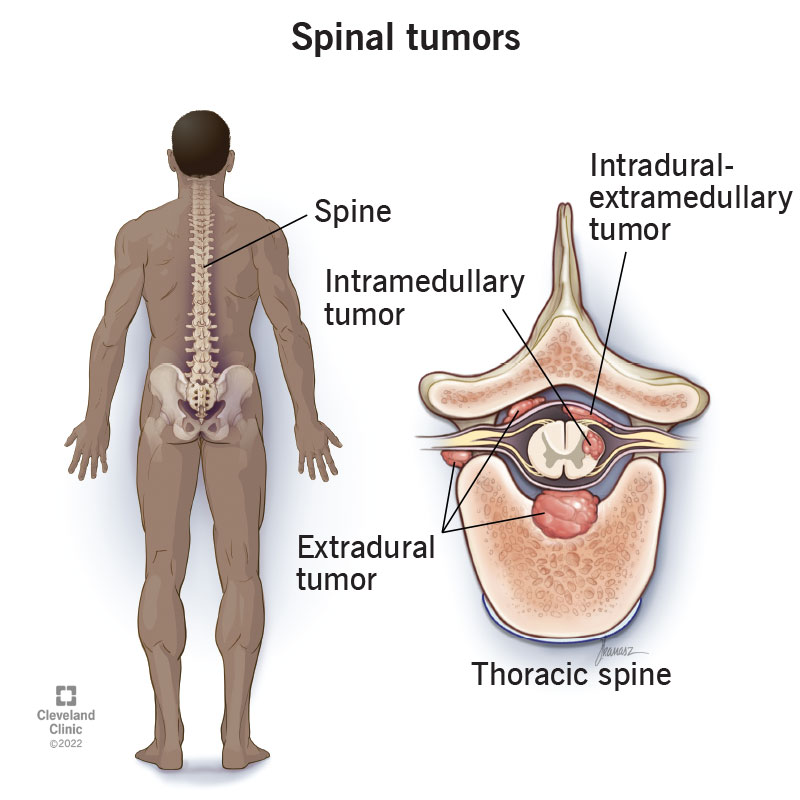
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17500-spinal-tumors)
A spinal tumor is an abnormal growth (mass) of cells within or surrounding your spinal cord and/or spinal column.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your spine (backbone) is the long, flexible column of bones that protects your spinal cord. It begins at the base of your skull and ends in your tailbone, which is part of your pelvis.
Your spinal cord is a cylindrical structure that runs through the center of your spine, from your brainstem (the bottom of your brain) to your low back. It contains nerve bundles and cells that carry messages from your brain to the rest of your body, and from your body to your brain.
Spinal tumors can be located:
Spinal tumors can be benign (noncancerous) or malignant (cancerous). If the tumor continues to grow, it can cause damage to different tissues in your spinal column.
Tumors that first develop on your spine or spinal cord are called primary spinal tumors. Metastatic, or secondary spinal tumors, result from cancer spreading from another area in your body to your spine. Metastatic spinal tumors are much more common than primary spinal tumors.
Healthcare providers categorize spinal tumors in many ways, including:
Advertisement
The different regions of your spine include:
While you can have a spinal tumor in any of these regions, the thoracic and lumbar regions are the most common locations.
Healthcare providers also describe spinal tumors based on where they form within your spinal column.
Since your spinal column is a complex structure that consists of several different types of cells and tissues, there are several types of spinal tumors, some of which include:
Advertisement
Common cancers that begin elsewhere in your body and can spread (metastasize) to your spine include:
These cancers most commonly metastasize (spread) to the bony part of your spinal column.
Anyone can get a spinal tumor, but they’re more likely to develop in people who have cancer, especially lung, breast and prostate cancers. These are considered metastatic, or secondary, spinal tumors.
Primary spinal tumors are rare but are more likely to occur in adults between the ages of 65 and 74 and in children between the ages of 10 and 16.
Secondary (metastatic) spinal tumors are common — they represent 97% of all spinal tumors. Every year, approximately 10,000 people in the United States develop metastatic spinal cord tumors. Studies show that 30% to 70% of people with cancer will experience cancer metastasis to their spine.
Advertisement
Primary spinal tumors, which begin in your spine, are uncommon. Benign (noncancerous) primary spinal tumors account for 0.5% of all newly diagnosed tumors. Malignant (cancerous) primary spinal tumors are even less common.
The symptoms of spinal tumors depend on several factors, including:
Some spinal tumors cause no symptoms because they’re small enough to not press on and irritate nearby tissues. However, as a tumor grows, it can cause certain symptoms, especially pain.
Back pain is the most common symptom of both benign (noncancerous) and malignant (cancerous) spinal tumors. Pain from spinal tumors in your middle or lower back is more common, as tumors are more likely to develop in those regions of your spine.
Pain from a spinal tumor usually:
Advertisement
Spinal tumors can also cause radicular pain, which is pain that radiates (spreads) from your spine to your hips, legs, feet or arms. Radicular pain often feels sharp and shooting.
Depending on the location and type of the spinal tumor, other signs and symptoms in addition to pain can develop. This usually happens when the tumor grows and presses on your spinal cord or your nerve roots, blood vessels or bones of your spine.
Other symptoms of spinal tumors include:
The cause of a spinal tumor depends on what type it is — primary or secondary (metastatic).
Scientists aren’t sure of the cause of most primary spinal tumors. Some of them may be caused by exposure to cancer-causing chemicals or substances. Spinal cord lymphomas (cancers that affect a type of immune cell) are more common in people with weakened immune systems. Spinal tumors can sometimes run in families, so scientists think there’s likely a genetic component.
By definition, secondary (metastatic) spinal tumors are caused by cancer that formed elsewhere in your body and spread (metastasized) to your spine.
Metastases most commonly develop when cancer cells break away from the main tumor and enter your bloodstream or lymphatic system. These systems carry fluids around your body, so they can carry cancer cells from one area of your body to another.
Metastases can also develop when cancer cells from the main tumor, typically in your abdominal cavity, break off and grow in nearby areas, such as in your liver, lungs or bones.
Since your spine has a significant blood supply and is near lymphatic and venous drainage systems, it’s generally vulnerable to metastasis.
As primary spinal tumors often have no symptoms (asymptomatic), healthcare providers often find them incidentally (accidentally) when a person is getting an imaging test for another reason.
People with symptomatic spinal tumors often believe that their back pain is related to a real or suspected injury in the recent past. If you’re experiencing back pain, it’s important to see your healthcare provider, especially if you have cancer.
Your healthcare provider will ask about your symptoms and medical history. They’ll also perform a neurological examination to check for the following symptoms:
Your healthcare provider will also order certain tests to help confirm or rule out a tumor diagnosis.
In addition to a physical and neurological exam, your healthcare provider may order several tests to confirm the presence of a spinal tumor, including:
Treatment of spinal tumors is very individualized and depends on the location, size and type of tumor. The goals of metastatic spinal tumor treatment include:
The goal of primary spinal tumor treatment is to remove the tumor completely if it’s causing symptoms, when possible.
Several different healthcare specialists are usually involved in the treatment plan for spinal tumors. These specialists may include:
Treatment options for spinal tumors vary depending on what type of tumor it is.
Your healthcare team may use a combination of therapies to treat a metastatic spinal tumor, including:
If you have a benign primary tumor that’s asymptomatic or mildly symptomatic and doesn’t appear to be changing or progressing, your healthcare provider may recommend monitoring it with regular MRIs.
Some primary spinal tumors can be surgically removed through complete en bloc resection (complete removal of the tumor) for a possible cure. But for other tumor types, particularly those that form inside the spinal cord-intramedullary, complete surgical removal isn’t possible without significant neural damage.
If your spinal tumor is malignant, you’ll need cancer treatments like the options listed above.
The prognosis (outlook) of spinal tumors depends greatly on your age and overall health and on whether the tumor is benign or malignant and primary or metastatic. Your healthcare team can give you a better idea of what to expect if you have a spinal tumor. Don’t be afraid to ask them questions.
In general, early diagnosis and treatment of a spinal tumor usually lead to a better outcome. If you’re experiencing symptoms of spinal tumors, such as back pain that gets worse at night, it’s important to see your healthcare provider.
Prevention methods for spinal tumors depend on the type — primary or secondary (metastatic).
Unfortunately, primary spinal tumors aren’t preventable.
In a small number of cases, primary spinal tumors may result from having certain genetic conditions, including:
If you have a first-degree family member (sibling or parent) with one of these conditions, it’s important to get genetic counseling or testing to see if you may also have the condition. Catching spinal tumors in their early stages generally has the best outcome.
Unfortunately, not all cases of secondary (metastatic) spinal tumors are preventable. Many people are diagnosed with metastatic cancer as their initial diagnosis.
The best way to try to prevent secondary spinal tumors is with adjuvant or neoadjuvant therapy if you’ve received a localized cancer diagnosis. The goal of adjuvant therapy is to shrink the primary tumor and prevent tumor cells that have broken away from the original tumor from forming metastatic tumors later on.
Healthcare providers use several different types of adjuvant therapy and are currently researching new types of treatment.
If you have a spinal tumor, it’s important to follow your treatment plan so it works as well as possible. You’ll also need support for the physical, emotional and social effects of living with back pain and/or cancer if these situations apply to you.
If you develop severe back that is sudden or gets worse, it’s important to see your healthcare provider, especially if you have a history of cancer.
Go to the nearest emergency room or call 911 if you develop new or worsening symptoms during treatment of a spinal tumor.
Learning that you have a tumor in your spine is scary. But know that your healthcare team will develop an individualized and thorough treatment plan to help relieve pain and improve your quality of life. Regular follow-up appointments after cancer treatment can help catch spinal tumor metastases early. Contact your healthcare provider if you develop symptoms of a spinal tumor.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
A spinal tumor can be a life-changing diagnosis. Cleveland Clinic’s experts will help you choose the best treatment plan while providing compassionate care.
