Overview

An estimated 5 million Americans have hernias and only 700,000 have them surgically repaired each year. While some hernias don't cause symptoms and no treatment is needed, some patients may avoid treating their hernias because they fear painful surgery. Often, however, hernia surgery is performed on an outpatient basis with a minimal recovery period.
Each year, Cleveland Clinic surgeons perform more than 3,000 hernia repairs affording patients expertise in both common and complex cases. More importantly, patients complete a comprehensive evaluation with a board-certified surgeon to determine the best surgical procedure to avoid repeat hernias and complications.
Why choose Cleveland Clinic's Comprehensive Hernia Center?
- Our patient-centered care is available at 17 locations across Northeast Ohio, making routine treatment more convenient for local patients. Our main campus in Cleveland is a destination for the most complex cases.
- Cleveland Clinic surgeons specialize in all types of hernia repair from the traditional, open technique to laparoscopic or minimally invasive surgery.
- Each year, we perform more than 3,000 hernia repairs , including:
- Inguinal hernias, which can be repaired laparoscopically on an outpatient basis.
- Incisional hernias, which may require a one or two day hospital stay.
- Ventral hernias, many which can be repaired with minimally invasive technique.
- Complex open and repeat surgeries – including abdominal wall reconstruction – which are referred to us from all over the world. We are able to perform successful repairs on patients who have lost most of their abdominal wall due to trauma or infections, tumor resection or multiple failed hernia repairs.
- We offer specialized programs including the Chronic Groin Pain Clinic, so patients don't have to live with chronic groin pain that may occur after Inguinal hernia repair surgery. The clinic offers a multi-disciplinary team approach, in collaboration with Pain Management, to determine which treatment options patients may respond to. Patients can get evaluated, including imaging, in one visit at the Chronic Groin Pain Clinic.
What We Treat
Cleveland Clinic’s Comprehensive Hernia Center treats a wide range of hernias, both common and complex:
- Ventral hernia – including umbilical, epigastric, incisional, parastomal, and multiply recurrent hernias.
- Hiatal hernia.
- Inguinal hernia.
- Paraesophageal/diaphragmatic hernia.
- Chronic groin pain after inguinal hernia repair.
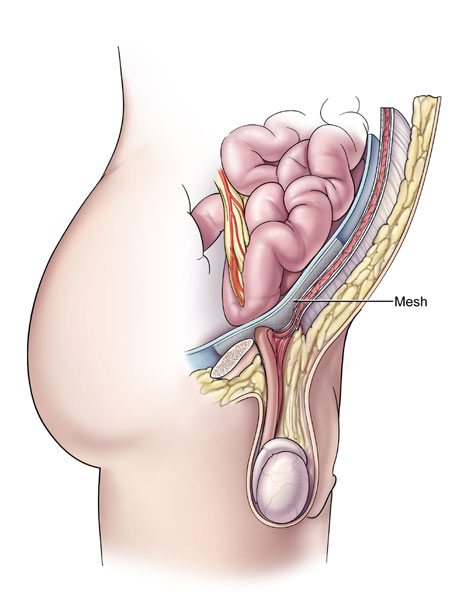
- Complications related to mesh – including mesh infection, fistula.
- Complex open and repeat surgeries – including abdominal wall reconstruction.
Treatments
Each year, while an estimated 5 million Americans develop hernias, only 700,000 have them surgically repaired. Most physicians believe people avoid treating their hernias because they fear painful surgery. Today, there is little reason to fear. Hernia surgery is usually performed on an outpatient basis and patients are able to return to most normal activities in a matter of a few days.
What is a hernia?
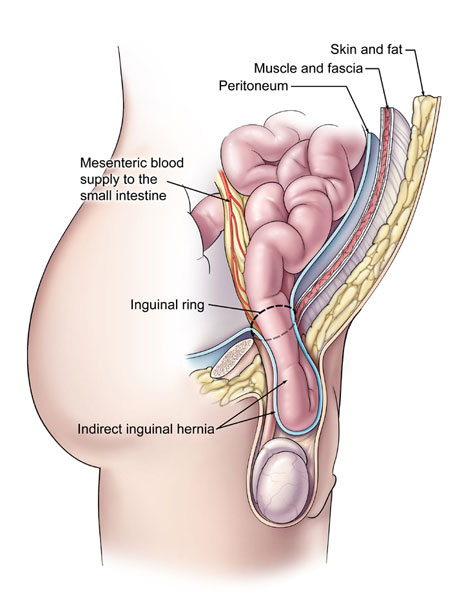
A hernia occurs when the inside layers of the abdominal wall weaken then bulge or tear. The inner lining of the abdomen pushes through the weakened area to form a balloon-like sac. This, in turn, can cause a loop of intestine or abdominal tissue to slip into the sac, causing pain and other potentially serious health problems.
Men and women of all ages can have hernias. Hernias usually occur either because of a natural weakness in the abdominal wall or from excessive strain on the abdominal wall, such as the strain from heavy lifting, substantial weight gain, persistent coughing, or difficulty with bowel movements or urination. There are three primary types of hernias:
- Incisional or ventral: appears at the site of the incision of a previous abdominal operation. This can happen soon after the operation or many years later.
- Inguinal: develops when a portion of an internal organ such as the intestine, along with fluid, bulges through a weakened area in the muscle wall of the abdomen.
- Umbilical: occurs around the navel and is usually present at birth, though it may not become a problem until adulthood.
What are the symptoms of hernias?
- A noticeable protrusion in the groin area or in the abdomen.
- Feeling pain while lifting.
- A dull aching sensation.
- A vague feeling of fullness.
How can a hernia be repaired?
Hernias usually need to be surgically repaired to prevent intestinal damage and further complications. The surgery takes about an hour and is usually performed on an outpatient basis (which means the patient can go home the same day of the procedure). This surgery may be performed by an open repair (small incision over the herniated area) or by laparoscopic surgery (minimally invasive) and in some case using robotic surgery (minimally invasive). Your surgeon will determine the best method of repair for your individual situation.
Open Ventral Hernia Repair
A ventral hernia is a hernia that occurs along the vertical center of the abdominal wall.
Innovations
Cleveland Clinic hernia experts have developed and currently use
- Newer minimally invasive methods.
- Leading-edge approaches to complex abdominal wall reconstructions, including robotic surgery and special techniques to prevent raising skin flaps.
- Novel methods of resection involving complex defects.
Some of these innovations have reduced post-operative infections and wound complications by more than 50 percent.
Images
FAQ
How soon can I return to work?
It depends on what type of work you do and which type of surgery you have. Typically, open repair patients may go back to deskwork within a week depending on how well you feel. Similarly, with laparoscopic repair, you may go back to deskwork within a few days.
If heavy lifting is required (greater than 20 – 25 lbs.), open repair patients may restrict this activity for 4 to 6 weeks. Patients with laparoscopic repair usually can begin heavy lifting in two weeks.
When can I resume normal activity?
Normal activity (minus exercise other than walking) for both open and laparoscopic repair can be resumed as soon as you feel well – usually within a few days.
Do I need a referral?
No, you do not need a referral to come to Cleveland Clinic. However, your insurance may require a referral. Be sure to check with your health care provider prior to your appointment.
How long does the surgery take?
Between one to two hours.
What causes a hernia?
A hernia occurs when the inside layers of the abdominal wall weaken then bulge or tear. The inner lining of the abdomen pushes through the weakened area to form a balloon-like sac. This, in turn, can cause a loop of intestine or abdominal tissue to slip into the sac, causing pain and other potentially serious health problems. Specifically, eighty percent of all hernias are located near the groin. Hernias may also be found below the groin (femoral), through the navel (umbilical) and along a previous incision (incisional).
How do I know if I have a hernia?
You may experience any of the following symptoms:
- A noticeable protrusion in the groin area, or in the abdomen.
- Feeling pain while lifting.
- A dull aching sensation.
- A vague feeling of fullness.
How is a hernia treated?
If a hernia causes no symptoms, you and your physician may choose to watch and see if any changes occur. A binder or support may be recommended for comfort, but does not treat the hernia. Most often surgery is required.
Will my hernia reoccur?
Approximately 5 to 10% of hernias are estimated to re-occur depending on the type of hernia. By following your physician’s recommendations following surgery, you can greatly affect your healing process and ultimate outcome.
Are there risks in delaying my surgery?
Your physician will recommend the urgency of need for surgery. In some cases, if the bowel becomes trapped in the opening caused by weakened muscles, blood flow can be blocked; causing pain to increase and often requiring prompt surgery.
Appointments and Locations
Appointments
To make an appointment at any one of our comprehensive Hernia Center locations, please call 216.444.6644.
If you are a MyChart patient, you may log in and make your appointment request from your MyChart account.
Locations
Resources
Butts and Guts podcasts
- Understanding Abdominal Wall Hernias and Options for Reconstruction – Ajita Prabhu, MD
- Chronic Groin Pain – David Krpata, MD
Health Essentials
- Why It's Important to Get Your Hiatal Hernia Fixed Right the First Time
- Can Heavy Lifting Give You a Hernia?
- Do Hernias Always Need to be Fixed?
- How You Can Get Relief from Groin Pain After Hernia Repair
Patient stories
Meet Our Team
Search for a Cleveland Clinic Surgeon Specializing in Hernia Repair in Our Find a Provider Tool
Find a ProviderFor Medical Professionals
What Is the Physiologic Tension of the Abdominal Wall?
Lead Surgeon: Benjamin T. Miller, MD
- Total Enrollment: 100 patients.
- Status: Currently Enrolling Patients.
- Estimated Enrollment Period: January 2022 – June 2022.
- ClinicalTrials.gov Identifier: NCT05163184.
- https://clinicaltrials.gov/ct2/show/NCT05163184?term=NCT05163184&draw=2&rank=1
How Does Tension on the Abdominal Wall Change After Hernia Repair?
Lead Surgeon: Benjamin T. Miller, MD
- Total Enrollment: 100 patients.
- Status: Currently Enrolling Patients.
- Estimated Enrollment Period: December 2021 – June 2022.
- ClinicalTrials.gov Identifier: NCT05142761.
- https://clinicaltrials.gov/ct2/show/NCT05142761?term=NCT05142761&draw=2&rank=1
Comparing Transfascial Sutures for Mesh Fixation to No Mesh Fixation in Open Retromuscular Repairs
Lead Surgeon: Ajita S. Prabhu, MD
- Total Enrollment: 325 patients.
- Status: Completed enrollment/long-term follow-up ongoing.
- Estimated Enrollment Period: October 2019 – March 2023.
- ClinicalTrials.gov Identifier: NCT03938688.
- https://clinicaltrials.gov/ct2/show/NCT03938688?term=NCT03938688&draw=2&rank=1
Is Extended Totally Extraperitoneal Repair for Ventral Hernia Superior to Intraperitoneal Onlay Mesh Repair (IPOM)?
Lead Surgeon: Clayton C. Petro, MD
- Total Enrollment: 100 patients.
- Status: Completed enrollment/long-term follow-up ongoing.
- Enrollment Period: November 2019 – November 2021.
- ClinicalTrials.gov Identifier: NCT04150796.
- https://clinicaltrials.gov/ct2/show/NCT04150796?term=NCT04150796&draw=2&rank=1
Does LiquiBand Mesh Fixation for Laparoscopic Inguinal Hernia Repair Reduce Postoperative Pain?
Lead Surgeon: Michael J Rosen, MD.
- Total Enrollment: 284 patients.
- Status: Completed enrollment/long-term follow-up ongoing.
- Multi-institutional study.
- Estimated Enrollment Period: July 2019 – July 2022.
- ClinicalTrials.gov Identifier: NCT04009213.
- https://clinicaltrials.gov/ct2/show/NCT04009213?term=NCT04009213&draw=2&rank=1
- Industry Sponsor: Advanced Medical Solutions Ltd..
Does Anterior Gastropexy Reduce Recurrence Follow Laparoscopic Paraesophageal Hernia Repair?
Lead Surgeon: Clayton C. Petro, MD.
- Total Enrollment: 240 patients.
- Status: Currently Enrolling Patients.
- Estimated Enrollment Period: June 2019 – December 2024.
- ClinicalTrials.gov Identifier: NCT04007952.
- https://clinicaltrials.gov/ct2/show/NCT04007952?term=NCT04007952&draw=2&rank=1
Does Pre-Operative Inguinal Nerve Injection of Local Anesthetic Predict Improvement in Chronic Groin Pain Following Neurectomy?
Lead Surgeon: David M. Krpata, MD.
- Total Enrollment: 50 patients.
- Status: Currently Enrolling Patients.
- Submitted to ClinicalTrials.gov, ID number pending..
Selected published or completed trials:
|
Effect of Hernia Mesh Weights on Postoperative Patient-Related and Clinical Outcomes After Open Ventral Hernia Repair: A Randomized Clinical Trial
|
|
Biologic vs Synthetic Mesh for Single-Stage Repair of Contaminated Ventral Hernias: A Randomized Clinical Trial
|
|
The Effect of Intraoperative Urinary Catheter on Postoperative Urinary Retention After Laparoscopic Inguinal Hernia Repair: A Randomized Control Trial
|
|
Comparing Sugarbaker Versus Keyhole Mesh Technique for Open Retromuscular Parastomal Hernia Repair
|
|
Robotic Inguinal vs Transabdominal Laparoscopic Inguinal Hernia Repair: The RIVAL Randomized Clinical Trial
|
|
2-Year Follow up to Robotic Inguinal vs Transabdominal Laparoscopic Inguinal Hernia Repair: The RIVAL Randomized Clinical Trial
|
|
Patient-Reported Outcomes of Robotic vs Laparoscopic Ventral Hernia Repair With Intraperitoneal Mesh: The PROVE-IT Randomized Clinical Trial
|
|
2-Year Follow-up to Patient-Reported Outcomes of Robotic vs Laparoscopic Ventral Hernia Repair With Intraperitoneal Mesh: The PROVE-IT-2 Trial
|
|
A Multi-Center, Prospective Clinical Trial of a Hepatic Derived Porcine Surgical Mesh for the Laparoscopic Repair of Symptomatic Paraesophageal Hernias
|
Clinical trials team
Director
Michael J. Rosen, MD
Staff surgeons
Cleveland Clinic Main Campus
- Michael J. Rosen, MD
- Ajita S. Prabhu, MD
- Clayton C. Petro, MD
- Lucas R. Beffa, MD
- Benjamin T. Miller, MD
- Steven Rosenblatt, MD
Fairview Hospital
- Diya Alaedeen, MD
- Kevin Baier, MD
Hillcrest Hospital
- David M. Krpata, MD
South Pointe Hospital
- Christian Massier, MD
Cleveland Clinic Florida (Weston)
- Emmanuelle Lo Menzo, MD
- Sam Szomstein, MD
Trial coordination
- Adele Costanzo, RN
Data analytics
- Jie Dai
Statistical analysis
- Chao Tu, MS
Center for Clinical Research
- Joan Booth, RN
- June Cassano
Current research fellows
- Katherine Montelione, MD
Incoming research fellows
- Sara Maskal, MD
- Ryan C. Ellis, MD
Clinical residents
- Aldo Fafaj, MD
- Samuel Zolin, MD
- Chase J. Wehrle, MD