Sleep apnea causes you to stop breathing while asleep. Your brain tries to protect you by waking you up enough to breathe, but this prevents restful, healthy sleep. Over time, this condition can cause serious complications. However, it’s manageable. A healthcare provider can help you get better sleep.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Sleep apnea is a condition that makes you stop breathing while you’re sleeping. This happens either because of blockage of your airway (obstructive sleep apnea) or because your brain doesn’t control your breathing as expected (central sleep apnea).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A lack of oxygen activates a survival reflex that wakes you up just enough to resume breathing. While that reflex keeps you alive, it also interrupts your sleep cycle. This prevents restful sleep. It can also put stress on your heart that may be life-threatening if untreated.
A healthcare provider can create a treatment plan to help you manage symptoms and prevent complications.
There are three types of sleep apnea:
One study estimates that about 1 billion people (between ages 30 to 69) around the world have obstructive sleep apnea. Central sleep apnea is less common than OSA but it’s not a rare condition.
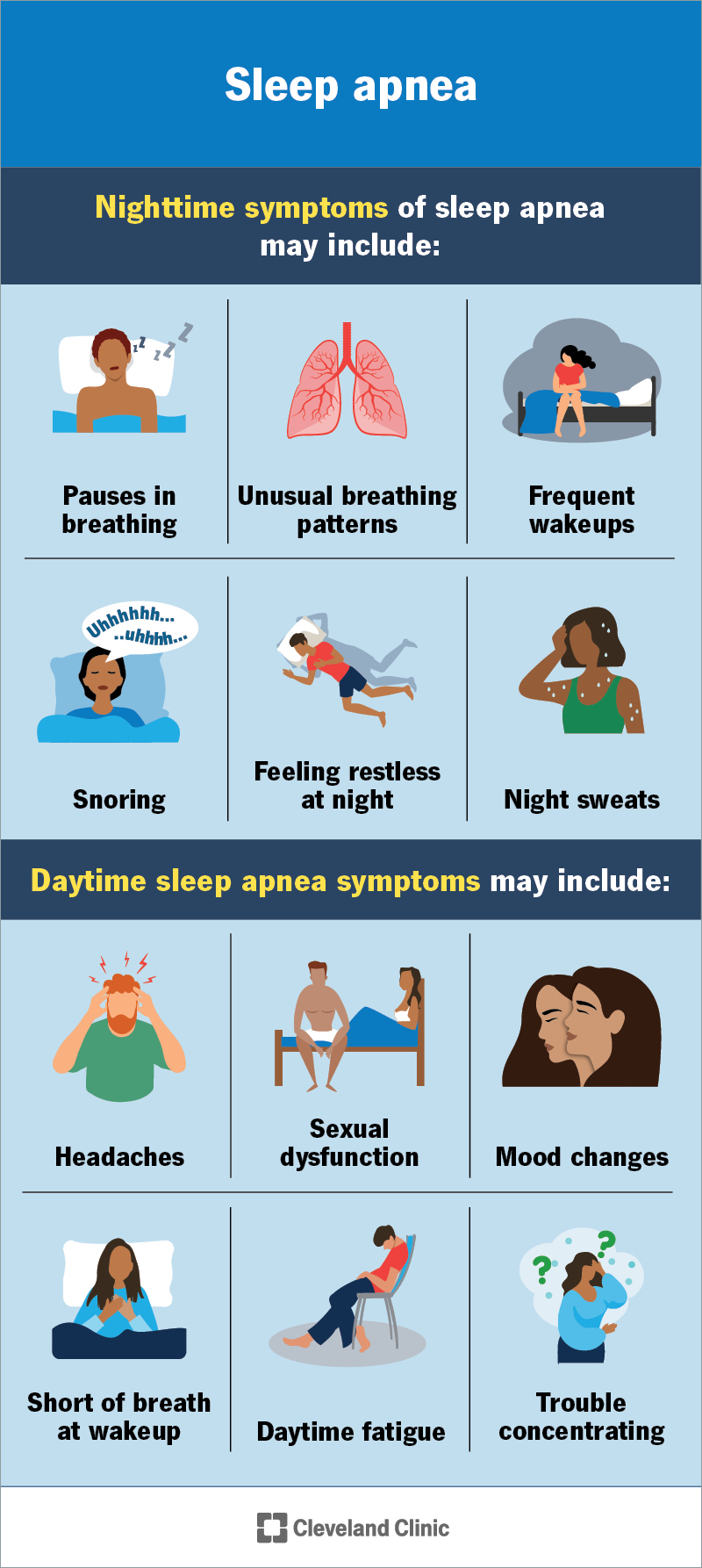
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/sleep-apnea)
Common symptoms of sleep apnea include:
Advertisement
Other symptoms you might experience may include:
Sleep apnea may look different in children.
Sleep apnea happens because of:
Anyone can develop this condition. It affects children and adults. Some common risk factors of sleep apnea include having:
Your risk increases as you get older. Males are more likely to receive a diagnosis before age 50.
Also, while you have a higher risk of sleep apnea with obesity, anyone of any body size can develop this condition.
Sleep apnea may cause several different complications, many of which are severe or life-threatening. These include:
A healthcare provider will diagnose sleep apnea by asking you questions about your symptoms and medical history. If they suspect the condition, they’ll recommend testing to confirm a diagnosis.
The most common tests for sleep apnea include:
If you suspect you or a loved one has sleep apnea, you might be able to help a healthcare provider diagnose it. Video and audio recordings of yourself or this person sleeping, especially where the provider can hear breathing, can give a provider key evidence they need to speed up the diagnostic process. You might also show evidence of air movement by holding a piece of tissue in front of a loved one’s face to make this movement visible on a recording.
Healthcare providers use the apnea/hypopnea index (AHI) to determine the severity of a sleep apnea diagnosis. The AHI measures the average hourly number of apnea (when you stop breathing while asleep) and hypopnea (decreased airflow) events. The severity levels of sleep apnea are:
Advertisement
What organ does sleep apnea affect?
Sleep apnea isn’t limited to only one organ in your body. In fact, it affects many different body systems. The two most affected include your circulatory system (heart) and nervous system (brain).
A healthcare provider will recommend different treatment options based on the type of sleep apnea and the severity. These may include:
Surgeries on your nose, mouth and throat may help prevent airway blockages during sleep. These surgeries include:
Advertisement
There isn’t a cure for all types of sleep apnea. For example, weight loss or surgical treatment options may cure obstructive sleep apnea. Your provider can give you more information about what this might look like for your situation.
Sleep apnea is a condition that can severely disrupt your sleep. You may not perform at your best during the day if you’re not getting restful sleep at night. This may put you at risk of injury or accidents that can interfere with your work, hobbies or social activities.
This condition can also cause complications that may be life-threatening. A healthcare provider can help you find the right treatment option that works for you. You may need to try a couple of different options or combinations to see what works best.
Sleep apnea complications may reduce your life expectancy if untreated. A healthcare provider will work with you to manage the condition and prevent this.
Many factors go into determining your life expectancy, so your provider is the best person to talk to about your situation since it may or may not match statistics.
You can’t prevent all causes of sleep apnea. But you can take steps to reduce your risk by:
Advertisement
There are several key steps you can take to manage this condition:
You should go to the emergency room if you notice any symptoms of the following:
If you recently received a sleep apnea diagnosis, you may want to ask your provider:
You might not know you have sleep apnea unless a sleep partner notices abnormal breathing patterns and tells you about them in the morning. You instead might be wondering why you’re not getting restful sleep each night. Sleep apnea is a common but manageable condition.
A healthcare provider may offer different treatment methods to see which ones work best for you, as treatment can vary from person to person. It may be challenging to change your sleep routine, but start small and perfect one change before moving on to another. Your provider may have other recommendations specific to your situation to help you get restful sleep each night.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Obstructive sleep apnea can keep you from the getting the good night’s rest you need. Cleveland Clinic’s experts can create a treatment plan that helps.
