Jaw surgery (orthognathic surgery) corrects misaligned jaws. It can treat conditions like TMJ disorders, malocclusion (“bad bites”) and obstructive sleep apnea. It’s a complex process that requires a lot of downtime. But it has a success rate of nearly 94%. Your dental provider might recommend jaw surgery when nonsurgical treatments aren’t enough.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
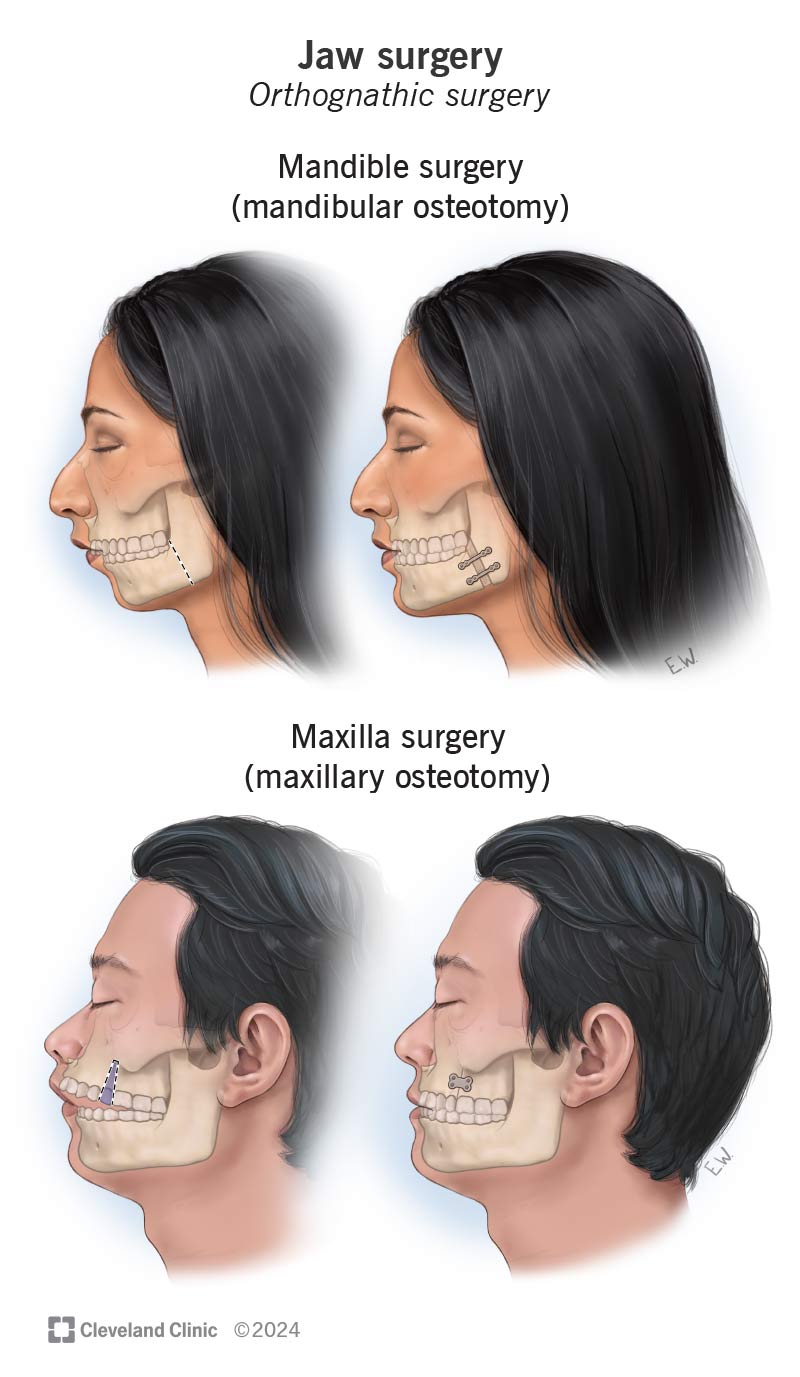
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/jaw-surgery.jpg)
Corrective jaw surgery (orthognathic surgery) changes the structure of your jawbone and brings your upper and lower jaws into proper alignment. Misaligned jaws can negatively impact your bite and make eating and speaking more difficult.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Jaw surgery isn’t a single event. It’s a two- to three-year process that combines surgery and orthodontics. Specifics vary for everyone, but here are the basics:
While there are some exceptions, most people can’t have jaw surgery until their jaws stop growing — usually in the late teenage years.
The three main types of corrective jaw surgery are:
Oral and maxillofacial surgeons or other head and neck surgeons use jaw surgery to treat:
Advertisement
You might need jaw reconstruction surgery after an accident or injury. This procedure may involve placing jaw implants to restore your appearance.
You’ll probably be on a liquid diet for about a month after your procedure. So, it’s a good idea to stock up on things like soups, smoothies, soft fruits and cooked vegetables you can liquefy using a blender.
Arrange for a trusted friend or family member to drive you to and from your appointment. You’ll be under anesthesia and will need someone to accompany you.
You can also make things easier on yourself if you get your medications filled at the pharmacy in advance. That way, when you come home from your jaw surgery, you’ll already have everything you need.
Before beginning your surgery, a healthcare provider will give you general anesthesia. That means you’ll be asleep and shouldn’t feel pain during the procedure.
What happens next varies depending on your unique situation. In general, during orthognathic surgery, your surgeon will:
Corrective jaw surgery is a complex procedure. It can take anywhere from one to four hours to complete.
You might go home the same day as your jaw surgery. But you’ll probably need to stay in the hospital for one to three days. During this time, your healthcare team will make sure that you’re healing as expected.
Following jaw surgery, it’s normal to develop side effects like:
These side effects should ease up after a week or two. Most people can return to work or school after three to four weeks. If you have pain that doesn’t go away with medication, let your surgeon know.
Orthognathic surgery can correct conditions that nonsurgical treatments can’t. For example, braces can move your teeth into new positions. But they can’t move your jaw or change its shape.
Jaw surgery is a complex procedure. But it’s the only way to change the skeletal structure of your mouth.
Orthognathic surgery has a success rate of around 93.9%. Most people who have it report an improved quality of life.
Like any major surgery, corrective jaw surgery comes with risks and possible complications.
General risks after surgery are:
Advertisement
Complications specific to jaw surgery could include:
Initial jaw surgery recovery should take about six weeks. But your jaw will continue to heal over the next several months. It might be a year before your jaw heals completely.
Every person’s recovery is different, but most people can resume light activity — like brief walks — after the first week or two. Talk to your healthcare provider before adding any exercise to your daily routine.
Here are some tips that can help during jaw surgery recovery:
Advertisement
Call your surgeon right away if you develop:
Jaw surgery is a major surgery that can disrupt your life for several weeks and months. But it can significantly improve your quality of life. If you’re thinking about jaw surgery, it’s important to be sure of your decision. Learn how recovery will affect your life so you can make plans. You owe it to yourself. Talk to your healthcare providers about your options and expectations. They’ll understand you’re making a big decision and will be glad to answer your questions. Just as important, they’ll give you time to be sure jaw surgery is right for you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s oral and maxillofacial surgery experts can help repair problems with your mouth, teeth and jaw with personalized treatment.
