Parasomnias are disruptive behaviors or events that affect your sleep. You might walk, talk or make physical movements to act out a dream. You might wake up in fear or be unable to move. There are a variety of parasomnias and treatment options available to help you fall asleep and stay asleep.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
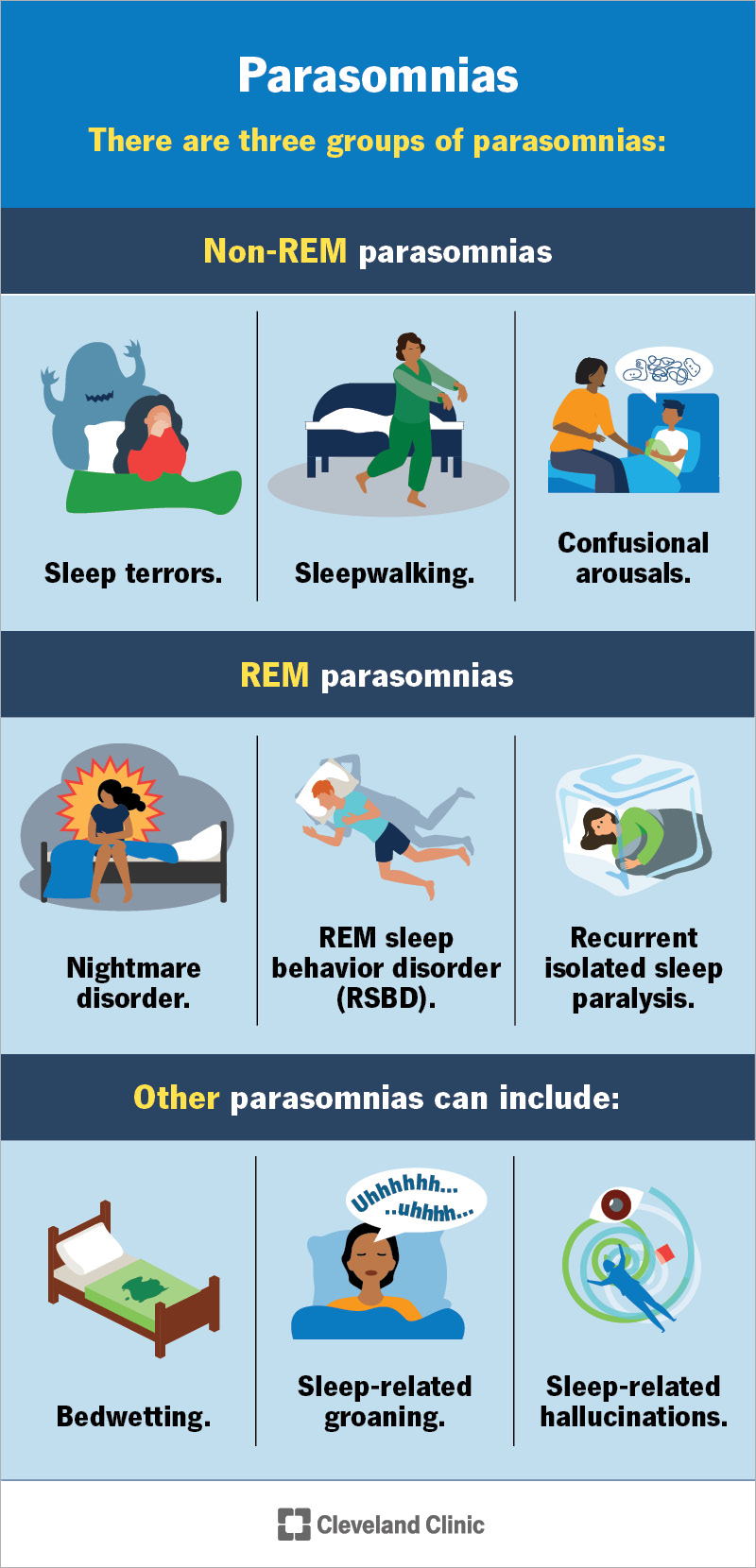
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/parasomnias)
Parasomnias are a type of sleep disorder that causes abnormal experiences or behaviors during sleep. These can happen as you’re falling asleep, during sleep or right before you wake up.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
If you have a parasomnia, you might:
When these events occur, others may think you’re awake, but you’re actually asleep. In the morning, you might not remember what you did while you were sleeping.
There are three main groupings of parasomnias based on the stage of sleep in which they happen.
Non-REM sleep parasomnias
The types of non-REM sleep parasomnias include:
Advertisement
REM sleep parasomnias
The types of REM sleep parasomnias include:
Other parasomnias
Parasomnia types that don’t fit into non-REM and REM sleep categories include:
Some parasomnias are more common than others. Since there are a variety of types, one study estimated that 4% to 67% of adults around the world experienced parasomnia in their lifetime.
Parasomnia symptoms vary based on the type but could include:
There are several possible causes of parasomnias. Your symptoms may be the result of something interfering with your ability to sleep through the night, like:
Certain medications can disrupt your sleep cycle and lead to parasomnia including:
Advertisement
There are several medical conditions that can cause parasomnia symptoms. Common conditions include:
Other common conditions or events that can cause parasomnia include:
Triggers are things that cause symptoms to happen. Triggers for parasomnia are different for each person but may include:
Parasomnias can affect anyone at any age. Children and young adults between ages 5 and 25 are more likely to develop non-REM parasomnias. Parasomnias in children usually happen with neurologic or psychiatric health conditions like epilepsy, attention-deficit/hyperactivity disorder (ADHD) or developmental challenges.
Advertisement
REM parasomnias most often affect people during adulthood. They usually appear alongside an underlying neurological or degenerative brain condition.
You may be more at risk of non-REM parasomnias if someone in your biological family has one.
Complications of parasomnia may include:
It’s very rare for parasomnias to cause fatal physical injuries.
A healthcare provider, usually a sleep specialist (somnologist), will diagnose parasomnia after a physical exam, neurological exam and testing.
During the exam, your provider will learn more about your symptoms. They may ask your bed partner or others who observed your behavior while you sleep to describe what they noticed. They’ll take a complete medical history and your family medical history, and they’ll learn more about what medications or supplements you currently take. Your provider will also ask you if you use alcohol or any non-prescribed drugs or substances, since those can affect your sleep.
Your provider will likely ask you to keep a sleep diary for at least one week. This is a record of when you go to bed, when you fall asleep, when you wake up and if you experienced any events or symptoms. A sleep diary is helpful for your provider to learn more about your sleep patterns.
Advertisement
Testing can help your provider rule out conditions with similar symptoms and narrow down the cause. Tests for parasomnias could include:
There isn’t a single cure for all parasomnias. Treatment is available to help you manage symptoms throughout your life. Many children notice parasomnias reduce or go away as they get older.
Treatment can vary based on each type of parasomnia. But all parasomnias can benefit from the following:
Your healthcare provider will discuss the best treatment options for your specific type of parasomnia considering your unique health history and any underlying medical conditions.
Medications that treat parasomnias include:
Your provider might prescribe medications for REM parasomnias but most likely not for non-REM parasomnias unless they’re long-lasting or potentially harmful. Medications aren’t the first line of treatment for parasomnias but they can be effective if proper sleep hygiene and bedtime habits don’t resolve your symptoms.
Some childhood parasomnias don’t need treatment since they resolve on their own as your child gets older.
Children who experience parasomnias may wake up scared, confused or anxious. Offering calming reassurance and reminding your child that everything is OK may help manage occasional parasomnias. But let their pediatrician know if parasomnias happen frequently and affect your child’s ability to function during the daytime.
Medications are rarely necessary, but if they are, they’re typically only prescribed for three to six weeks. Common medications include benzodiazepines or anti-anxiety medications.
It’s normal to experience occasional parasomnias like nightmares throughout your life. Sometimes, sleep disturbances happen frequently and interfere with your ability to stay awake during the daytime and function as expected.
Each person’s experience with parasomnia is different. A child may outgrow certain nighttime behaviors or natural aging could bring on more sleep disturbances. No matter what situation you’re in, if you’re not getting the rest you need to feel well during the daytime, a healthcare provider can help you.
Treatment options are available and range from changing your sleep routine to taking medications regularly. Your provider may modify the medications you take if parasomnia is a side effect.
You can’t prevent all causes of parasomnias, such as those from neurological diseases, mental health conditions or genetics. The best way to reduce your risk of parasomnias is to practice good sleep hygiene. Also, ask your healthcare provider to review your current medications. Many can disrupt sleep. If this is the case, your provider may offer an alternative medication to avoid side effects.
Your healthcare provider may offer tips to keep you safe if you experience parasomnias, like sleepwalking or REM sleep behavior disorder, where injury during sleep is possible. Tips may include:
Visit a healthcare provider if:
If anything about your sleep routine is concerning, let a provider know. They can help you get the sleep your body needs.
You may want to ask your provider:
You might not know or remember what you did or dreamt about while you were sleeping. Most often, someone who shares your living space may be the first to notice parasomnia events. These events might happen a few times during your lifetime. But they could occur every night or multiple times per week. It can be stressful and emotionally taxing to be unable to get the rest you need each night. When your behaviors put your daytime activities and wakefulness at risk, it’s time to talk to a healthcare provider. Treatment is available for parasomnia to help you fall asleep and wake up rested without disturbances.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Yelling, kicking, walking and even eating in your sleep can be serious. When you have parasomnias, Cleveland Clinic’s sleep experts can help.
