Sleep paralysis is when you can’t move right before falling asleep or waking up. It’s temporary. As you sleep, your brain helps the muscles in your arms and legs relax. With sleep paralysis, you’re stuck between sleep phases. Finding the source of your symptoms and addressing them can help you avoid future episodes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Sleep paralysis is when you can’t move any part of your body right before falling asleep or as you wake up. It happens when your body is in between stages of sleep and wakefulness. An episode is temporary and only lasts for a few seconds to a couple of minutes. It’s a type of parasomnia.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You’ll likely feel scared or anxious during a sleep paralysis episode. When it ends, you may feel confused because you’ll regain movement of your body as if nothing happened.
Even one sleep paralysis episode can make you nervous about going to sleep. This can affect how you feel and function during the daytime.
There’s no treatment available to stop a sleep paralysis episode when you’re in the middle of one, but treatment is available to reduce how often episodes affect you.
Sleep paralysis isn’t dangerous, but it can cause emotional distress during an episode. Some cases of sleep paralysis link to other sleep disorders, so let a healthcare provider know if you’re not sleeping well.
An estimated 30% of people around the world experience at least one sleep paralysis episode within their lifetimes.
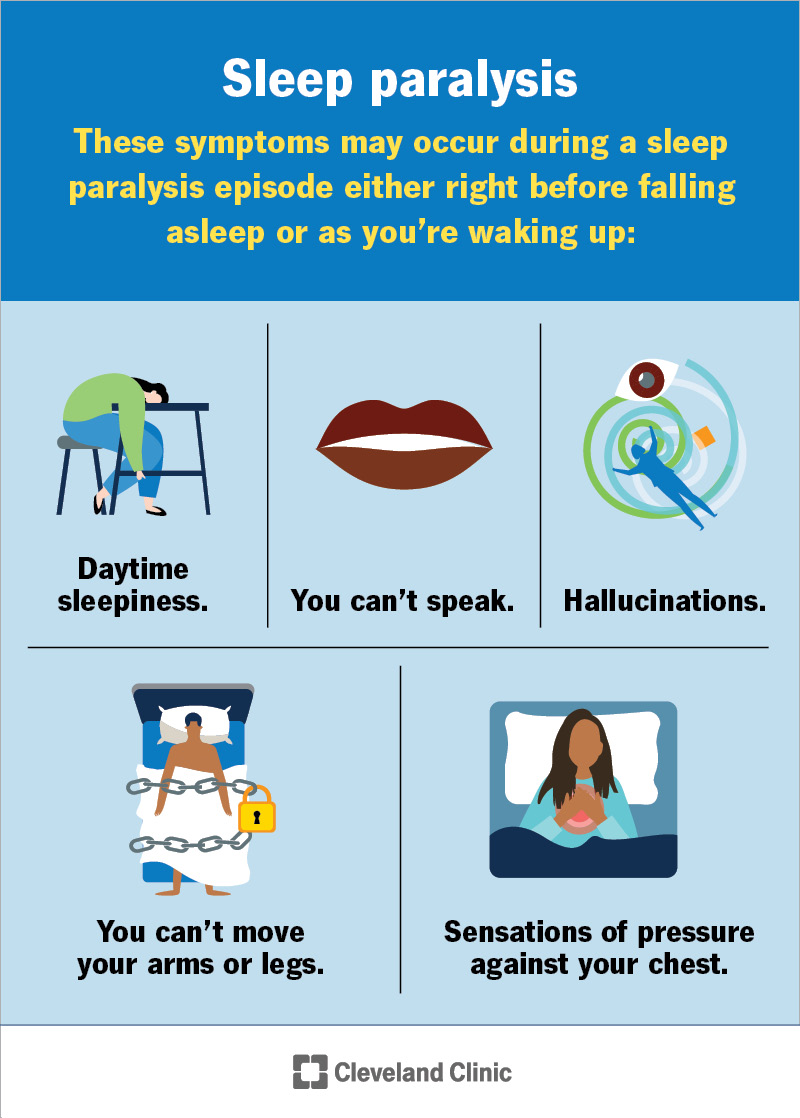
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21974-sleep-paralysis)
You may experience the following symptoms during a sleep paralysis episode either right before falling asleep or as you’re waking up:
During a sleep paralysis episode, you’re aware of your surroundings but can’t move or speak. You can still move your eyes and breathe. You may feel:
Advertisement
The length of time you’ll experience a sleep paralysis episode varies. It could only last for a few seconds or up to 20 minutes. It usually only lasts a couple of minutes.
You can safely wake someone up during a sleep paralysis episode. The person having an episode may wake up fully and regain movement when you touch or talk to them. Someone in a sleep paralysis episode won’t be able to tell you what they feel or indicate with movement that they’re having an episode until they’ve recovered from one.
The exact cause of sleep paralysis is unknown. Healthcare providers notice they could happen with the following:
Sleep paralysis happens when you regain awareness going into or coming out of rapid eye movement (REM) sleep. Your body hasn’t fully switched sleep phases or woken up during sleep paralysis.
When you’re sleeping, your brain sends signals that relax the muscles in your arms and legs. The result — muscle atonia — helps you remain still during REM sleep. As you’re in the REM sleep stage, you’ll likely have dreams. Your brain prevents the muscles in your limbs from moving to protect yourself from acting dreams out and causing injury.
Sleep paralysis can happen to anyone at any age. It’s more common among people who have a varying sleep schedule (like with shift work). Symptoms may first appear in childhood or adolescence. Episodes are more frequent in your 20s and 30s.
Healthcare providers confirm or rule out sleep paralysis after a physical exam and a sleep evaluation. Your provider may ask you about:
Your healthcare provider may recommend testing if they suspect a sleep disorder that causes sleep paralysis like narcolepsy. You may need:
Advertisement
Your treatment will depend on the reason why you have sleep paralysis. Your provider may recommend the following:
There’s no way to stop a sleep paralysis episode as it happens. You may notice that you come out of an episode sooner if you focus on making small body movements, like moving one finger, followed by moving two fingers, etc.
You may experience only one episode in your lifetime. But this varies from person to person. You’re more likely to have an episode during periods of high stress or when you’re not sleeping well.
It’s natural to feel tired, confused and scared after a sleep paralysis episode. Sleep paralysis is a frightening experience. Be kind to yourself, including getting extra rest if you need it. Talk to a loved one for comfort or see your healthcare provider if you have concerns.
There isn’t much you can do to prevent sleep paralysis from happening. But there are steps you can take to lower your risk.
Advertisement
One of the best ways to avoid sleep paralysis is to improve the quality of your sleep. You can do this by:
If you have frequent sleep paralysis episodes, you should discuss them with your healthcare provider. There may be an underlying cause that they can treat.
Questions you may want to ask your provider include:
Sleep paralysis can leave you feeling worried and scared after an episode. When you regain movement, you might wonder what caused this to happen or if it’ll happen again. The experience could’ve felt so strange that you may wonder whether anyone will believe you. These feelings can prevent you from getting quality rest at night and feeling well enough to perform at your best during the day.
If sleep paralysis is a concern, don’t let these feelings hold you back from getting medical attention and the support you need. A provider can pinpoint the causes, provide treatments or offer self-care recommendations to lower your risk of future episodes.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Yelling, kicking, walking and even eating in your sleep can be serious. When you have parasomnias, Cleveland Clinic’s sleep experts can help.
