An atrial septal defect (ASD) is a congenital heart defect that involves a hole in the atrial septum. This is the muscular wall that separates the two upper chambers (atria) of the heart. Small ASDs usually don’t need treatment. Larger ones may require percutaneous (nonsurgical) repair or surgery to lower the risk of serious complications.
An atrial septal defect (ASD) is a hole in the atrial septum, which is the wall that separates your heart’s two upper chambers (atria). An ASD is a congenital heart defect (something you’re born with) that happens when the septum doesn’t form properly. It’s also called a “hole in the heart.”
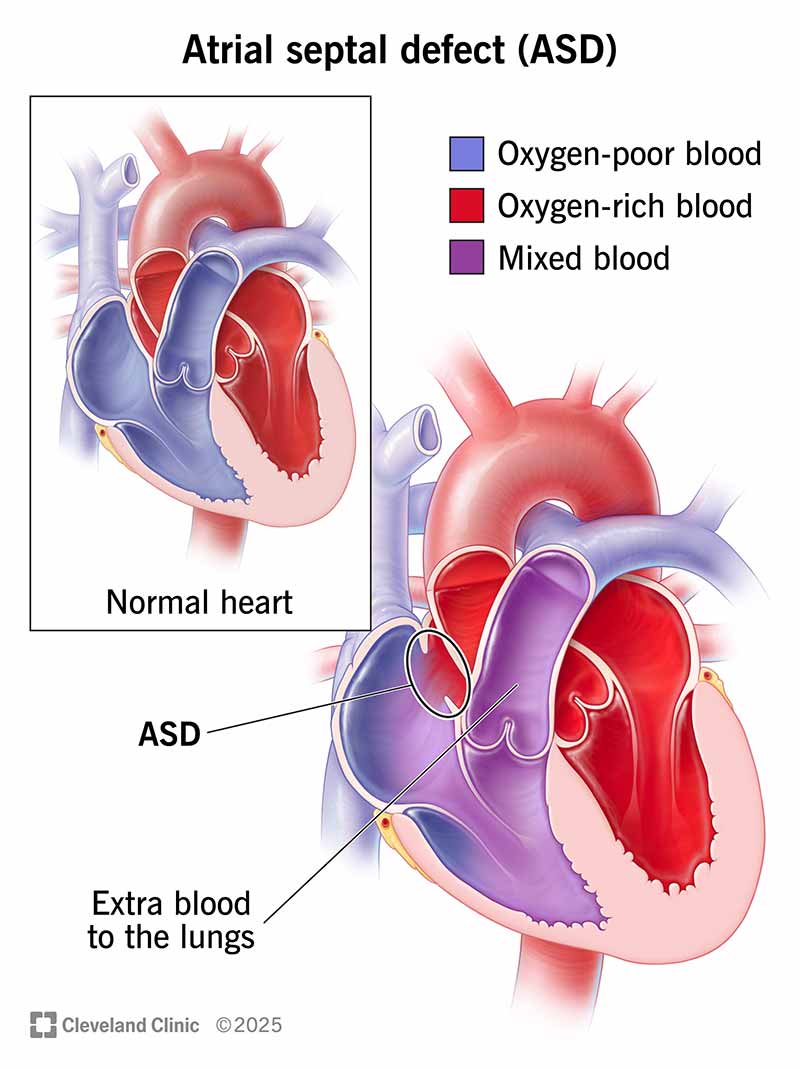
An ASD allows an abnormal shunt, meaning an abnormal passageway for blood that shouldn’t be happening. Normally, oxygen-rich blood flows from your left upper chamber (atrium) down to your left lower chamber (ventricle), and then out to supply oxygen to your body. An ASD causes some blood from your left atrium to flow in the wrong direction, into your right atrium. Your right atrium contains oxygen-poor blood that needs to cycle through your lungs. So, your right atrium now has extra blood that ultimately goes to the lungs.
This wrong-way leak might be minor and not cause any problems. In those cases, the ASD can be left alone without treatment. Other times, it can lead to problems with your heart or lungs. The bigger the ASD, the more likely it is to cause symptoms and need treatment.
There are four main types of atrial septal defects. They’re defined by their location in the atrial septum.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An atrial septal defect is one of the most common types of congenital heart defects in children. It occurs in approximately 1 to 2 out of 1,000 live births. About 1 in 1,859 babies are born with an atrial septal defect in the U.S. This adds up to about 2,118 babies born with ASD each year.
Some babies born with an atrial septal defect also have other heart defects or genetic disorders. Some associated heart defects include:
Associated genetic disorders include:
An atrial septal defect (ASD) and a patent foramen ovale (PFO) are both openings in the atrial septum. But ASD is a congenital heart defect, meaning it’s a problem that occurred while a fetus was still in the uterus. Septal tissue should’ve formed in that part of the atrial septum, but didn’t. So a baby is born with a hole in their heart.
A patent foramen ovale isn’t a congenital heart defect. Tissue isn’t missing from the atrial septum. Instead, a PFO happens when a normal flap-like opening in a baby’s heart (foramen ovale) doesn’t seal shut after birth. The foramen ovale is normal, and we all have one when we’re born. This is a normal pathway to allow oxygen-rich blood from the placenta to circulate to the fetus’ brain while in the uterus.
When we’re born, we no longer need the foramen ovale since our lungs start working. So it usually closes on its own soon after birth and completely seals off in a couple of days or weeks after. When it doesn’t close on its own, it’s called a patent foramen ovale. “Patent” means open or failing to close.
A PFO is usually smaller than an ASD. That’s why it doesn’t usually cause any problems or symptoms. The risk of symptoms and problems goes up when an opening in the septum is bigger.
PFOs are much more common than ASDs. Estimates show that about 1 in 4 adults have a PFO. Most people never know they have this small opening in their hearts. It’s usually harmless, but people who have a PFO along with heart problems such as atrial fibrillation may face a higher risk of a stroke.
A small ASD doesn’t affect your body much. But larger ASDs can strain the right side of your heart. That’s because the right side of your heart now has extra blood it must pump out to your lungs. Plus, this extra blood flow can slowly damage the blood vessels in your lungs.
Problems with large ASD include:
Even though an atrial septal defect is present at birth, many people don’t have symptoms until far into adulthood. Small ASDs (less than 5 millimeters) may not cause symptoms because they don’t strain the heart or lungs.
Most children have no signs or symptoms. The most common (and often the only) sign will be a heart murmur. Their healthcare provider will notice it when listening to their heart with a stethoscope.
When children do have other symptoms, they include:
Although extremely rare, children with larger ASDs may have symptoms that include:
Tell your child’s provider about any symptoms you notice. Their provider may want to run some tests to check your child’s heart structure and function.
Adults with ASD may feel symptoms by age 40. Symptoms depend on how much the ASD has strained the heart and lungs. They include:
If you have any of these symptoms, call your healthcare provider right away. These symptoms could mean you have an untreated ASD. Or, they could mean you have another cardiovascular problem that needs treatment. If you have chest pain, you should call 911 or your local emergency number.
The exact cause of atrial septal defects isn’t fully known. However, congenital heart defects are often caused by genetic changes that happen before birth. Some genetic mutations associated with ASD affect the NKX2.5/CSX and TBX5 genes.
Some factors can raise a birthing parent’s risk of having a baby with congenital heart disease. These factors include:
Atrial septal defects are diagnosed through a physical exam along with tests that check your heart’s structure and function.
Your provider will run one or more tests to diagnose you with an ASD and learn how it’s affecting your heart. These include:
In some cases, Cardiac CT scan or Heart MRI may be used. They’re most helpful for people with associated defects or less common forms of ASD.
Atrial septal defects can be closed through surgery or percutaneous (nonsurgical) repair.
The type and timing of ASD treatment depends on many factors, including:
Small ASDs usually don’t need repair. However, larger ASDs should be repaired even if they aren’t causing symptoms. This prevents serious complications down the road.
Once you have signs of heart or lung damage, repair is essential. Your provider will recommend treatment if:
Your provider may prescribe medications to treat some symptoms of ASD. But there aren’t any medications that can close the hole.
If you have pulmonary hypertension, you may need to take medication before your repair procedure. This medication treats pulmonary hypertension and makes the procedure safer for you.
This type of repair uses a device (called a septal occluder) to close the hole in your atrial septum. The device is put in place using a long, thin tube called a catheter. The occluder is attached to the catheter, which is guided to your heart through a vein in your groin. When the occluder is released from the catheter, it opens up and seals the hole. Over time, tissue grows over the occluder, and it becomes part of your heart.
Percutaneous repair can close most secundum ASDs and some sinus venosus ASDs. So, this is the method used most often.
Before the repair, you’ll have a cardiac catheterization to check the size and location of the ASD and measure pressures in your heart.
After the repair, you’ll take blood-thinning medication (anticoagulant or antiplatelet) to keep blood clots from forming on the device (a possible but rare complication). Your provider will talk with you about the right type of medication for you and how long you need to take it.
Surgery is needed for primary ASDs, coronary sinus defects and most sinus venosus ASDs. These are rare defects that require treatment by a cardiac surgeon with expertise in congenital heart disease. Robotic-assisted surgery or minimally invasive surgery may be options for some people.
A surgical repair usually involves using a tissue patch to close the ASD. The tissue often comes from your own pericardium (the membrane around your heart). Some secundum ASDs can be surgically closed with just sutures and no patch.
There’s no specific way to prevent atrial septal defects. They develop when a fetus is still in the uterus. But prenatal care may impact a fetus'schances of having congenital heart disease. If you’re pregnant or planning a pregnancy, it’s important to:
Genetic testing may be helpful if you or other biological family members have congenital heart disease.
People with an ASD may have a lower life expectancy than those without an ASD. Life expectancy depends on many factors, including the size of the ASD and whether you have ASD repair. The timing of repair also matters. Research shows that people who have ASD repair earlier in life have a better outlook. This is likely because early repair catches the problem early before it can cause serious damage to your heart or lungs.
People who need ASD repair but don’t have it by age 40 face the greatest danger. Their risk of death goes up by 6% with each passing year.
If you’ve been diagnosed with an ASD, it’s important to keep all your medical appointments and follow your provider’s guidance. Heart defects like ASD often call for “watchful waiting.” This means your provider keeps an eye on the situation to see when you need treatment. Your provider will tell you how often you need to come in for appointments.
If you’ve had ASD repair, you should follow your provider’s guidance for follow-ups. You’ll likely go back for follow-ups:
If your child has an ASD, their provider will let you know the next steps and when intervention might be needed. In general, small ASDs are treated with “watchful waiting.” Larger ASDs usually require procedures at a younger age to prevent problems later on. Talk with your child’s provider to learn more about the best treatment plan for them.
People with an atrial septal defect should follow their provider’s guidelines for at-home care and medical follow-ups. After ASD repair, you’ll likely have activity restrictions for a while as you recover. You’ll also need to take medications such as:
After you’ve recovered from ASD repair, it’s still important to do whatever you can to take care of your cardiovascular system. Work with your provider to learn how you can reduce your risk of future heart and vascular problems. Your provider may offer suggestions including:
Call your provider any time you have questions or concerns. Thanks to advances in diagnosis and treatment, people with ASDs have a good outlook for a fruitful and enjoyable life.
A note from Cleveland Clinic
Learning that you have a “hole in your heart” can be an alarming experience. It’s even scarier if this happens to your child. But there’s good news. Modern medical advances have made atrial septal defects much more treatable than they used to be. And some ASDs don’t even need treatment because they’re too small to cause problems.
Talk with your provider or your child’s provider to learn more about next steps. When possible, seek the advice and care of a congenital heart disease specialist at a high-volume hospital. These doctors can manage your individual needs with the most advanced treatment options.
Last reviewed by a Cleveland Clinic medical professional on 07/15/2022.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy