May-Thurner syndrome is a condition that affects blood flow. It occurs when the right iliac artery, which sends blood to your right leg, presses on the left iliac vein, which carries blood from your left leg to your heart. Some people have no symptoms of May-Thurner syndrome. Others develop deep vein thrombosis (DVT) or blood clots in the legs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
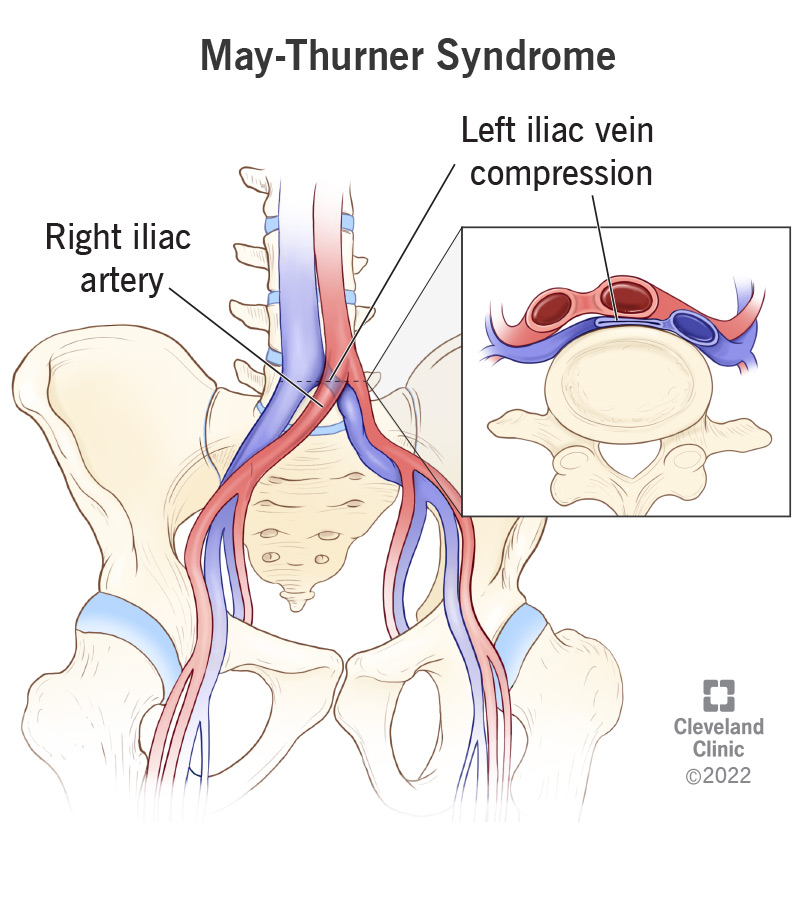
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17213-may-thurner-syndrome)
May-Thurner syndrome is when your right iliac artery presses on (compresses) your left iliac vein. Your right iliac artery is the main blood vessel that carries blood to your right leg. Your left iliac vein is the main blood vessel that carries blood from your left leg back to your heart. May-Thurner syndrome may interrupt typical blood flow through your legs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Other names for May-Thurner syndrome include:
May-Thurner syndrome makes it harder for blood to flow back to your heart. Instead, it may pool in your legs and can develop into deep vein thrombosis (DVT). DVT occurs when a blood clot forms in your deep leg veins. DVT symptoms may include:
Some females with May-Thurner syndrome may also develop pelvic congestion syndrome. Experts believe pelvic congestion syndrome occurs when problems with the veins in your pelvis cause chronic pelvic pain.
Your veins and arteries continually carry blood throughout your body. Your arteries take oxygen-rich blood from your heart and deliver it to the tissues throughout your body. When your tissues have received the oxygen and nutrients, your veins carry the oxygen-poor blood back to your heart and lungs.
Your veins and arteries cross over each other at some places in your body. Your right iliac artery crosses over your left iliac vein in your pelvis. This usually isn’t a problem. But in May-Thurner syndrome, the right iliac artery puts pressure on the left iliac vein. The effect is like stepping on a hose. Your left iliac vein compresses, and it’s harder for blood to flow freely through it.
Advertisement
May-Thurner syndrome is slightly more common in females. It’s also more common in adults ages 20 to 50.
Iliac vein compression is common, occurring in about 1 in 5 people. However, many people with iliac vein compression don’t have a formal diagnosis of May-Thurner syndrome. This may be partly because most people don’t have symptoms of May-Thurner syndrome unless they develop DVT.
Many people don’t have any symptoms of May-Thurner syndrome, especially if they don’t have DVT. Symptoms usually only affect your left leg and may include:
May-Thurner syndrome occurs because your right iliac artery presses on your left iliac vein. However, experts aren’t exactly sure why this compression happens.
May-Thurner syndrome diagnosis starts with discussing your health history and symptoms with your healthcare provider. Your provider conducts a physical exam and may use tests that look at your blood vessels, such as:
May-Thurner syndrome treatment focuses on improving blood flow and reducing your risk of developing DVT. Your provider may recommend:
If you have DVT due to May-Thurner syndrome, your provider may also recommend:
Advertisement
The main complication of May-Thurner syndrome is DVT. If a blood clot in your legs breaks off and travels to your lungs, it’s known as a pulmonary embolism.
A pulmonary embolism is a life-threatening medical emergency. Call 911 if you experience any new or worsening symptoms of a pulmonary embolism, including:
Many people live long, healthy lives with May-Thurner syndrome. You may not even know you have the condition if you don’t have any symptoms.
Call your healthcare provider if you experience any symptoms of deep vein thrombosis. Many people successfully treat DVT with medications.
There’s no way to prevent May-Thurner syndrome because experts don’t know what causes it. But you can improve your circulation and decrease your risk of blood clots by:
Advertisement
If you have May-Thurner syndrome or think you could, you may want to ask your healthcare provider:
May-Thurner syndrome can lead to a pulmonary embolism, which is a life-threatening complication. Call 911 immediately if you experience any symptoms of a pulmonary embolism.
You may not be able to tell if you have May-Thurner syndrome. Most people don’t know they have the condition unless they develop symptoms of DVT.
The only way to know for sure if you have the condition is to have imaging tests that show your right iliac artery compressing your left iliac vein.
May-Thurner syndrome occurs when your right iliac artery compresses your left iliac vein. This compression disrupts blood flow and may lead to DVT. Many people have no symptoms of May-Thurner syndrome. Others experience pain, swelling or feelings of heaviness in their legs. Treatment for May-Thurner syndrome focuses on relieving the pressure on your left iliac vein and restoring blood flow.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
