Clostridioides difficile, or C. diff, is a highly contagious bacterium that causes diarrhea and colitis. It often infects people who’ve recently taken antibiotics. Antibiotics that kill other bacteria in your gut but don’t kill C. diff allow it to quickly grow out of control. You have to take a different antibiotic to treat C. diff.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
C. diff is a nickname for a bacterium whose full name is Clostridioides difficile (klos-TRID-e-OY-dees dif-uh-SEEL). This bacterium can infect your colon (large intestine), causing diarrhea and other uncomfortable symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Bacterial infections in your colon are common, and most aren’t serious. But C. diff infection can be more aggressive and harmful to your colon. C. difficile releases toxins that damage the cells in your intestinal lining. This causes inflammation in your intestinal lining and colon (colitis). Whether you have symptoms, and how severe they are, will depend on the extent of the damage from these toxins. When it’s severe, it can be life-threatening.
Clostridioides difficile is a newer name for Clostridium difficile.
C. diff infection (CDI) is a global health concern, although the exact rates of infection worldwide are unknown. In the U.S., 500,000 infections cause 15,000 deaths each year.
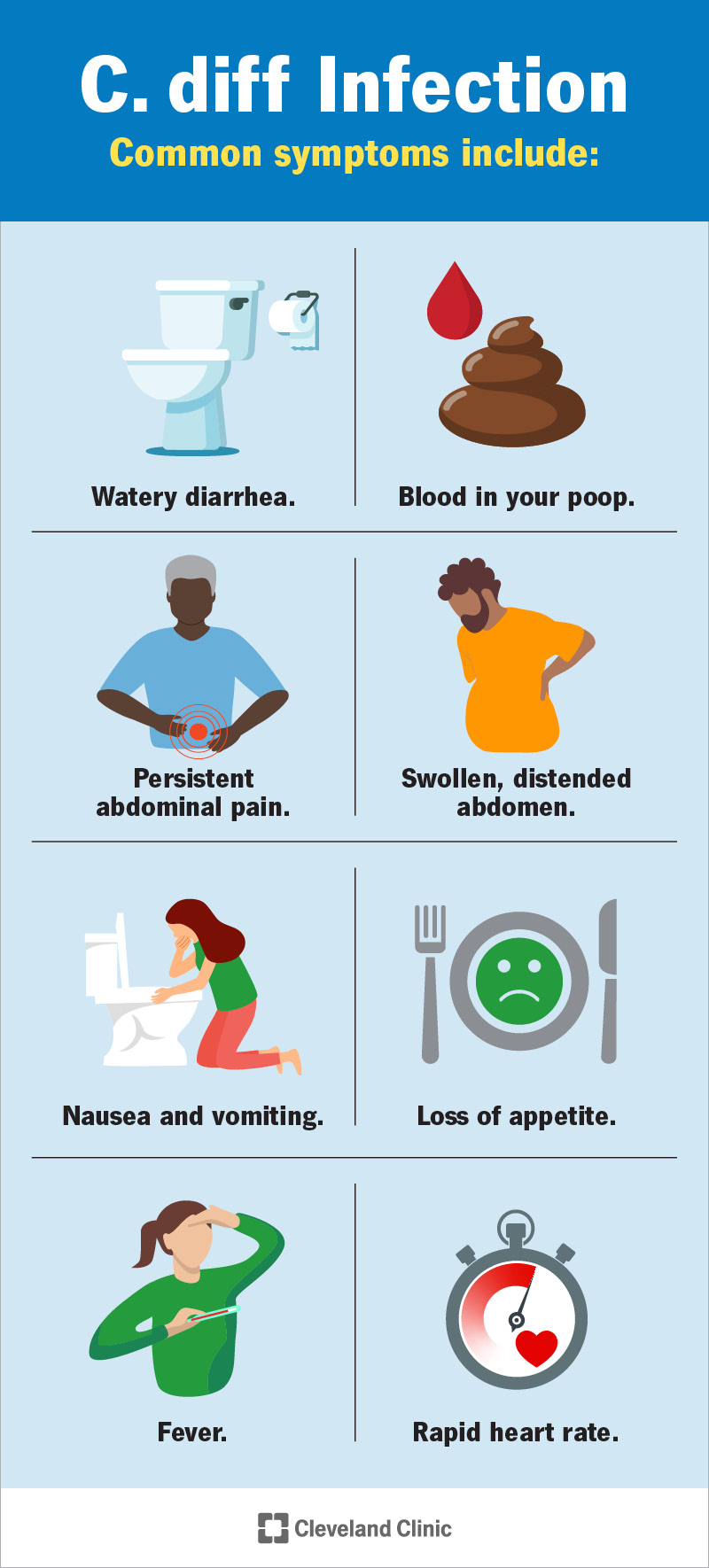
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15548-c-diff)
The most common symptom, and usually the first to appear, is watery diarrhea. A mild infection will cause diarrhea at least three times a day, often with some abdominal cramping.
As C. diff infection becomes more severe, diarrhea increases. It may occur as much as 10 to 15 times a day. You may notice traces of blood in your poop or other symptoms, like:
C. diff symptoms may resemble food poisoning or stomach flu at first. If you’re taking antibiotics, it’s possible to mistake C. diff diarrhea for a normal side effect of medication.
Advertisement
But sometimes, C. diff infections can occur without diarrhea.
C. diff diarrhea is typically mushy or porridge-like, but not completely liquid. Sometimes, it has a green tint, though other bacterial infections can also cause this. Occasionally, it contains blood, mucus or pus.
Many people notice a distinctive odor with C. diff diarrhea. They describe it as unusually strong and oddly sweet. This smell may be because C. diff increases the levels of bile acids in your poop.
A healthy immune system normally protects your gut from C. diff infection by keeping C. diff levels under control. If they grow out of control, it’s because something has affected the balance between “helpful” bacteria and “unhelpful” bacteria. Everyone has bacteria in their intestines. Helpful types of living bacteria help to keep other bacteria, like C. diff, in check.
The most common cause of C. diff infection is taking antibiotics. Using them upsets the balance between helpful and unhelpful bacteria in your gut microbiome, allowing C. diff to dominate and overgrow.
C. difficile reproduces by releasing spores. These spores can also spread on skin, surfaces and other items. This means if you touch something with the spores on it, and then eat or touch your mouth, you can get C.diff that way.
Outside your body, C. diff turns into spores that are very hard to kill, both inside and outside of your intestines. They’re resistant to heat, acid and many antibiotics and disinfectants. They can also survive for months on surfaces.
Researchers estimate about 5% of the population has C. difficile in their colon without signs or symptoms of infection. You can have C. diff under control, but still carry and spread it to others.
Yes, you can be around someone with C. diff if you take precautions. To minimize the risk of spreading the infection, you should:
Medical conditions that may reduce your defenses against C. diff infection include:
Advertisement
Other risk factors associated with C. diff infection include:
Sometimes, it isn’t clear what allowed C. diff to take over. While many factors can affect your gut immunity, it’s important to know that infection can occur even if you don’t have any known risk factors.
Complications can occur with more severe infections. How severe your infection becomes will depend on several factors, including the strain of the bacteria you have and how strong your immune system is.
People who have more risk factors for getting a C. diff infection in the first place may be more at risk of a severe infection. They may also have repeat infections, which cause more damage over time.
Common complications include:
Advertisement
As toxic damage in your colon progresses, you may have further complications, including:
If your healthcare provider suspects C. diff infection based on your symptoms, they’ll take a sample of your poop and send it to a lab. The lab will test it for C. diff toxins.
If you test positive, your healthcare provider may conduct further tests to find out how severe the infection is. These may include blood tests and imaging tests that look inside your colon.
Treatment for C. diff infection is based on how severe it is. If you developed a C. diff infection while taking antibiotics, your provider might begin by simply stopping those medications.
Advertisement
For some people, this is enough. Their natural gut immunity returns and overcomes the infection. If this doesn’t happen, your provider will prescribe antibiotics that can stop C. diff.
Antibiotics to treat C. diff include:
If you have a mild infection, you’ll take the prescription home with you. Most people will start improving in a few days. If your infection is more severe, you might need to stay in the hospital.
In the hospital, your provider might give you antibiotics through an IV, along with fluids to prevent dehydration. In some cases, they might deliver medications directly into your colon as an enema.
If you have severe complications, you might need intensive care. In rare cases, providers recommend emergency surgery to remove the source of the infection in your colon. This is called colectomy.
If you’ve recovered but you continue to have repeat infections after treatment, your options are:
Most C. diff infections are mild and go away with treatment. But the circumstances that cause C. diff infection sometimes allow it to spread very quickly. C. diff infection can be sudden and severe.
If you have risk factors that make you more vulnerable to C. diff infection, you may be more likely to have a more severe infection or have repeat infections and need more extensive treatment.
It can go away on its own if your healthy gut bacteria return to defeat it. This is more likely if your intestinal flora is normally strong and you don’t have any long-term health factors that usually weaken it.
If you got the infection because you were taking antibiotics, it might go away after you stop taking them. But don’t wait too long for this to happen. If you don’t feel better in a few days, contact your provider.
It’s likely that some of the bacteria will survive after treatment, but you can have some without having an infection. As long as helpful gut bacteria also survive, they should help to control C. difficile.
If you have repeat infections, it’s because these other bacteria haven’t been restored yet. Repeat infections may be the original one relapsing, but they aren’t always. Sometimes, they’re new infections.
The most common long-term problem is ongoing or repeat infection with C. difficile. This happens when your colon is having trouble recovering completely. Your colon may be slower to recover if:
More rarely, some people develop autoimmune disorders after a severe infection. This means that their immune systems continue to act as though they have an infection even when they don’t anymore.
Autoimmune disorders that start after C. diff infection include post-infectious IBS (irritable bowel syndrome) and reactive arthritis.
Healthcare providers take special precautions when dealing with C. diff infection to help prevent the spread of this highly contagious disease. You can follow their example to help keep others safe:
You might want to ask:
Clostridioides difficile is an ordinary bacterium, and it can live in your gut without doing harm. But when it starts taking over, it can be aggressive. You may feel worried about frequent diarrhea and how it’ll impact your life. Having a condition that affects your poop can be embarrassing to discuss. Don’t let these feelings stop you from seeking help.
Most people won’t have complications from C. diff, and it’ll go away quickly and completely. But it can become severe, especially if certain risk factors make you more vulnerable. It’s highly contagious and can be persistent, coming back again and again.
If you develop diarrhea after taking antibiotics, tell your healthcare provider. Don’t take anti-diarrhea medications, which won’t help and might make it worse. If you suspect you have C. diff, contact your provider right away.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
