Rheumatoid vasculitis is a type of vasculitis (blood vessel inflammation). It affects people who’ve had rheumatoid arthritis (RA) for a long time (usually 10 years or more). It causes skin rashes, sores and discoloration, usually on or around your fingers, hands, feet and toes. Managing RA can help reduce your risk of vasculitis and lessen its severity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
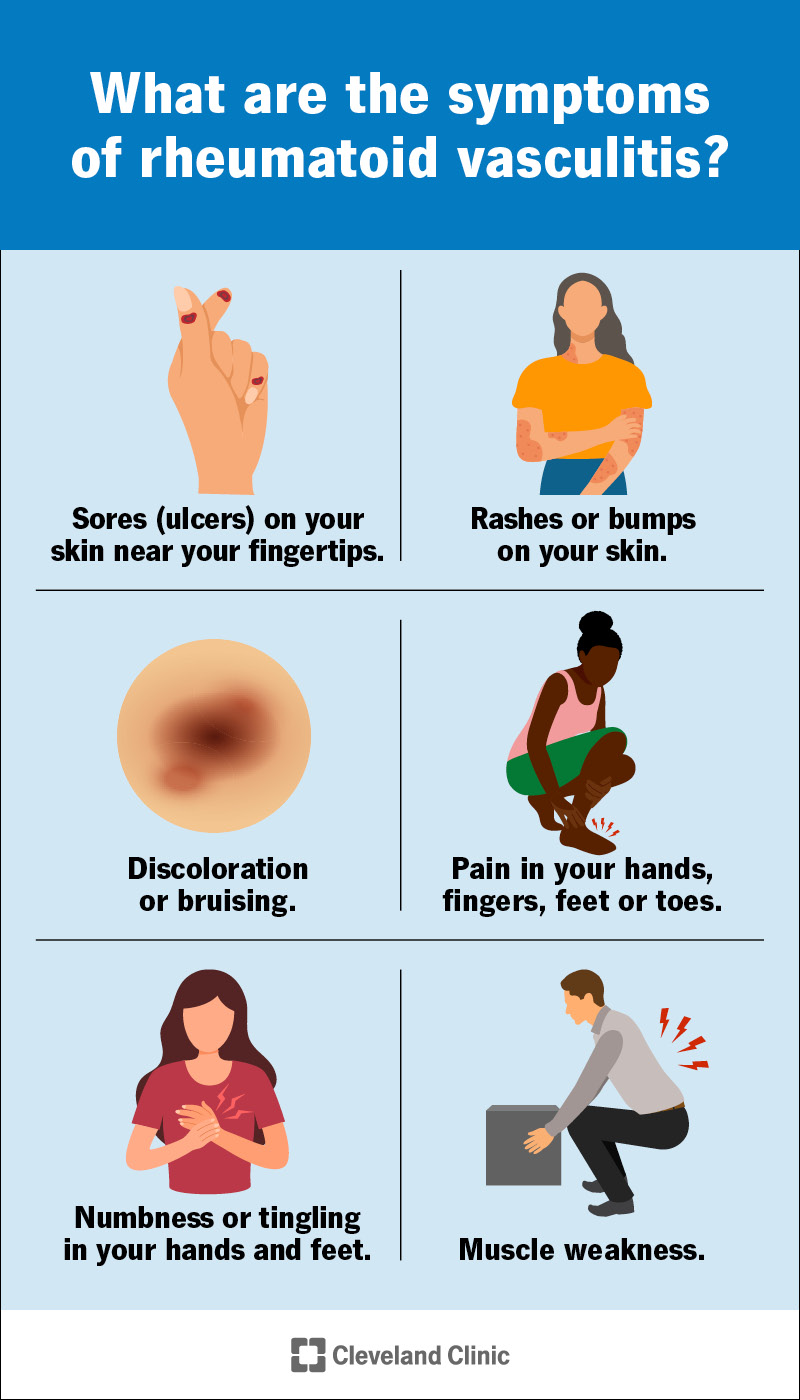
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/rheumatoid-vasculitis-infographic)
Rheumatoid vasculitis is a type of vasculitis that’s triggered by having rheumatoid arthritis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Vasculitis causes inflammation in your blood vessels. Blood vessels are channels that carry blood throughout your body. They form a circuit that begins and ends at your heart.
Rheumatoid arthritis (RA) is arthritis that happens when your body’s immune system damages tissue in your joints.
Rheumatoid vasculitis, RA and other types of vasculitis are all autoimmune diseases. Autoimmune diseases happen when your immune system accidentally attacks your body instead of protecting it.
Rheumatoid vasculitis is rare. Fewer than 50 out of every million people in the U.S. have it.
People older than 50 are more likely to develop rheumatoid vasculitis, but it’s still uncommon. Experts estimate that it affects fewer than 300 out of every 1 million people older than 50 in the U.S.
Rheumatoid vasculitis was more common in the past, but the number of cases has declined since researchers and healthcare providers developed more effective treatments for rheumatoid arthritis.
Some of the most common rheumatoid vasculitis symptoms include:
Advertisement
Severe cases of rheumatoid vasculitis can cause other symptoms, including:
Rheumatoid vasculitis is an autoimmune disease. It happens when your immune system attacks your blood vessels.
If you have severe rheumatoid arthritis (RA) for a long time (usually more than 10 years), your immune system might start damaging your blood vessels, especially in your hands and feet. The affected blood vessels swell and thicken, which makes it harder for blood to flow through them. Over time, the inflammation can damage the affected blood vessels and the skin they connect to.
Anyone with rheumatoid arthritis can develop rheumatoid vasculitis, but some people with RA have a higher risk, including those who have:
Rheumatoid vasculitis can cause severe complications if it’s not diagnosed and treated. These complications are rare, but can include:
A healthcare provider will diagnose rheumatoid vasculitis with a physical exam and some tests. They’ll ask you about your symptoms and when you first noticed them. Tell your provider how long you’ve had rheumatoid arthritis, and how you’re managing it.
Your provider might use a few tests to diagnose rheumatoid vasculitis, including:
You’ll probably need to see a rheumatologist — a healthcare provider who specializes in treating inflammatory diseases.
Your provider will suggest treatments to manage your symptoms. They’ll help you find treatments that prevent damage to your blood vessels and organs. Managing your rheumatoid arthritis symptoms can often treat rheumatoid vasculitis, too. Talk to your provider about which RA treatments you’re currently using, and if they suggest changing them.
If you do need specific treatments for rheumatoid vasculitis, your provider might suggest prescription medications, including:
Advertisement
Quitting smoking (and other tobacco products) can reduce the severity of rheumatoid vasculitis. It might also prevent rheumatoid vasculitis before it develops. Talk to your provider about smoking cessation options. They’ll help you find ways to quit safely and effectively.
You should expect to manage rheumatoid vasculitis for a long time, maybe for the rest of your life. Even if you don’t have severe symptoms, you’ll need to see a provider regularly to monitor any changes in your blood vessels. Ask your provider how often you need follow-up appointments and tests.
You can’t prevent rheumatoid vasculitis because you can’t prevent the rheumatoid arthritis (RA) that usually triggers it. There’s no way to know if (or when) someone will develop it.
If you have RA, managing it will reduce your risk of developing vasculitis. If you smoke, quitting may also decrease your rheumatoid vasculitis risk.
Monitor your symptoms and keep track of any changes you notice. Follow the treatment plan you worked on with your provider. Don’t hesitate to visit them if you think a treatment isn’t working (or isn’t as effective as it used to be).
See your provider if you notice new symptoms, or if your symptoms are getting more severe.
Advertisement
Your provider will tell you how often you’ll need regular follow-up appointments, tests or additional screenings.
You may want to ask your provider:
It can be extra frustrating to find out the rheumatoid arthritis you’ve been managing for years is causing inflammation in your blood vessels alongside all your joint symptoms. Your healthcare provider will help you find ways to tweak your RA treatment plan alongside any new medications you might need. They’ll tell you what to watch out for and how you can prevent complications.
Trust your instincts and listen to your body. The best way to prevent complications is to see your provider regularly. Don’t be afraid to talk to your healthcare provider about any new or changing symptoms you’re experiencing.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Rheumatoid arthritis is a chronic condition, but with the right treatment, you can manage it. Cleveland Clinic is here to help you live an active life.
