Scleroderma makes your body produce too much collagen, a protein that you need for healthy skin and tissue. It’s an autoimmune condition, which means your immune system attacks your body instead of protecting it. Scleroderma can cause lots of symptoms and affect tissue throughout your body. It can also lead to life-threatening complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
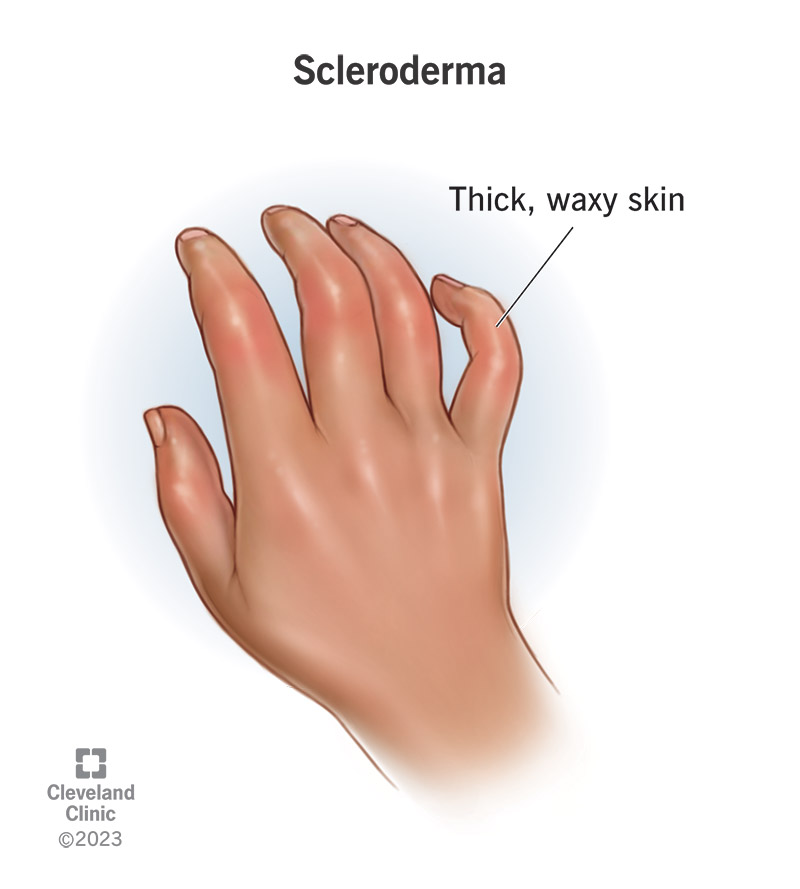
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/8979-scleroderma)
Scleroderma is a rare condition that makes your body produce tissue that’s thicker than it should be. Scleroderma usually affects your skin, but can cause symptoms in any tissue throughout your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Scleroderma is an autoimmune disorder. Autoimmune disorders happen when your immune system accidentally attacks your body instead of protecting it. Experts don’t know why your immune system turns on you. It’s like it can no longer tell the difference between what’s healthy and what’s not — between what’s you and what’s an invader like bacteria or a virus.
If you have scleroderma, your immune system triggers your body’s cells to produce too much collagen (a protein). Your body needs collagen to have strong, healthy connective tissue to support your organs and hold parts of your body in place. But when you produce too much of it, your skin and other tissue can be thicker and more fibrous than they should be.
Scleroderma is a chronic condition, which means you’ll need to manage your symptoms for a long time (maybe the rest of your life). It can also cause life-threatening complications if it affects tissue in your organs. Call 911 (or your local emergency services number) or go to the emergency room if you feel like you’re having a heart attack, can’t breathe or can’t swallow.
Visit a healthcare provider if you’re experiencing symptoms like pain and stiffness in your joints, especially if you notice thickened skin around your fingers and toes.
Advertisement
Healthcare providers classify scleroderma into two main types:
Localized scleroderma: Localized means concentrated in one area. Localized scleroderma only affects one part of your body (usually your skin). It causes thick patches or streaks on your skin that feel waxy. Localized scleroderma can get better (resolve) on its own. It usually doesn’t spread to other parts of your body.
Systemic sclerosis: Systemic sclerosis can affect other organs, in addition to your skin. It can affect parts of your respiratory system (the organs that help you breathe and smell) and your digestive system (the organs that help you turn foods and drinks into energy). Scleroderma is more likely to cause serious complications if it affects your ability to breathe or process nutrition. It can be fatal. Systemic sclerosis has three subtypes — diffuse, limited and sine sclerosis.
Diffuse means spread out widely. Diffuse sclerosis causes thickened skin over larger areas at once, including your:
It can also affect multiple organs at once, including your:
Healthcare providers usually refer to limited scleroderma with the acronym CREST syndrome. Each letter in CREST stands for a symptom it causes:
Sine sclerosis causes limited sclerosis symptoms, but doesn’t affect your skin. You may have any CREST syndrome symptoms but not experience any thickened skin.
Scleroderma is rare. Experts estimate that all types of scleroderma affect around 250 out of every 1 million people in the U.S. Around 100,000 people in the U.S. have systemic scleroderma.
Some people with early scleroderma don’t have any symptoms. The most common scleroderma symptom is having patches or streaks of thickened, waxy skin. Other common symptoms include:
Which other symptoms you experience (and where they affect you) depends on which type of scleroderma you have.
People with localized scleroderma usually only experience skin thickening. The thickened skin can be isolated to one specific area or appear in patches. It can affect skin on your:
Advertisement
It’s rare for localized scleroderma to affect your internal organs.
Systemic scleroderma can cause lots of symptoms. It causes thickened skin, usually in larger areas and patches, including on your face and hands. Thick skin usually appears on your fingers or toes and then spreads toward the center of your body. If you have Raynaud’s syndrome, the skin on your affected fingers and toes may change color when they’re exposed to cold (usually white, reddish or purple).
Systemic sclerosis can also cause symptoms in other organs and tissue, like your:
Advertisement
Experts don’t know for sure what causes scleroderma.
Some studies have found that it can run in families (meaning biological parents can pass it on to their children), but this is rare enough that there’s no definite proof it’s a genetic disorder.
Anyone can develop scleroderma, but some groups of people have a higher risk:
People with scleroderma are much more likely to have two other conditions: Raynaud’s syndrome and Sjögren’s syndrome.
Reynaud’s syndrome affects small blood vessels in your fingers and toes (your digits). People with it have episodes of symptoms (sometimes called attacks). It makes blood vessels in your digits suddenly tighten (contract) more than they should. This can make the skin in your affected digits turn pale or lighter than your natural skin tone. They might also look bluish.
Sjögren’s syndrome makes your body produce less moisture in certain glands — usually the salivary glands in your mouth and the glands in your eyes that produce tears. Some people with Sjögren’s syndrome experience muscle and joint pain, too.
Advertisement
Some types of scleroderma can cause severe complications, including:
Some of these complications can be fatal. Visit a healthcare provider as soon as you notice any new or changing symptoms. Call 911 (or your local emergency services number) or go to the emergency room if you think you’re experiencing a heart attack or feel like you can’t breathe or swallow.
A healthcare provider will diagnose scleroderma with a physical exam and some tests.
You might need to visit a rheumatologist, a healthcare provider who specializes in treating autoimmune disorders. They’ll examine your body and ask you about your symptoms. Tell your provider which symptoms you’re experiencing, when you first noticed them and if anything seems to make them worse.
You’ll also need a few tests to rule out other conditions that cause similar symptoms.
Diagnosing scleroderma is usually part of a differential diagnosis. This means your provider will probably use a few tests to determine what’s causing your symptoms before ruling out other conditions and diagnosing you with scleroderma. Some tests you might need include:
You’ll probably also need a few imaging tests to take pictures of the inside of your body, including:
There’s no cure for scleroderma, but your healthcare provider will help you find a combination of treatments that manages your symptoms and minimizes how much they impact your daily routine.
Which treatments you’ll need depends on where you’re experiencing symptoms and how severe they are. Some common scleroderma treatments include:
You should expect to manage scleroderma and its symptoms for the rest of your life. Even though there’s no cure, most people find treatments and lifestyle tweaks to minimize how much their symptoms impact their day-to-day lives.
Living with a chronic condition can be extremely frustrating. Ask your healthcare provider about additional resources like support groups or educational opportunities to help you manage stress and your mental health.
Because experts don’t know what causes it, there’s no way to prevent scleroderma.
In addition to your regular treatments, you might be able to manage some of your symptoms by making some changes in your daily routine, including:
Scleroderma can cause so many different symptoms that it’s sometimes hard to notice at first. Visit a healthcare provider if you notice any new pain or other symptoms, especially if they’re getting worse. Even if something else is causing your symptoms, a provider will diagnose the cause and suggest treatments to manage them.
Talk to your provider if you feel like your scleroderma treatments aren’t working as well or if your symptoms are changing or getting worse — especially if they affect your ability to breathe or swallow.
Call 911 (or your local emergency number) or go to the emergency room if you’re experiencing heart attack symptoms like chest pain, trouble breathing or you feel like you can’t swallow.
Most people with scleroderma don’t experience life-threatening complications.
You have a higher risk of severe complications if you have systemic scleroderma that affects your internal organs. Your healthcare provider will tell you what to expect and if you have an increased risk of fatal complications.
Any chronic condition is serious, including scleroderma. That’s because you’ll probably have to manage symptoms for the rest of your life. However, that doesn’t mean scleroderma will control your life. No two people’s experiences are the same. Share your concerns or worries with your healthcare provider.
Scleroderma can be a very frustrating condition to live with. Because experts aren’t sure what causes it and there’s no one treatment that works for everyone, it might take time to find treatments that manage your symptoms well. Your healthcare provider will help you at every step of the process.
Trust your instincts and your body if something feels “off.” Even subtle changes in your symptoms can be a sign of an issue your healthcare provider should examine. Don’t be afraid to ask them questions or share concerns about your symptoms or treatments.
Living with a chronic condition can be exhausting. Take time to give yourself credit and recognition for all the hard work it takes to manage your symptoms.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic takes a team approach to scleroderma treatment. We’ll help you slow its progression and manage your symptoms.
