Tension headaches are the most common headache type. Healthcare providers may call them tension-type headaches. These headaches may feel like pressure on your forehead and temples. There are home treatments for tension headaches, and healthcare providers may prescribe medication and other therapies that will ease tension headache pain and pressure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A tension headache is a headache that feels like there’s a tight band wrapped around your head that puts pressure on your forehead and temples. Healthcare providers may call them tension-type headaches. Many factors cause tension headaches, and you may be unable to avoid all potential triggers. Fortunately, there are many things you can do to prevent a tension headache. And if home treatment doesn’t work, healthcare providers may have medications and other therapies to ease tension headache pressure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthcare providers classify tension headaches based on how often you have one. Condition types include:
Tension headaches are the most common primary headache type. Researchers estimate more than 70% of people have episodic tension headaches. Females are more likely to get them.
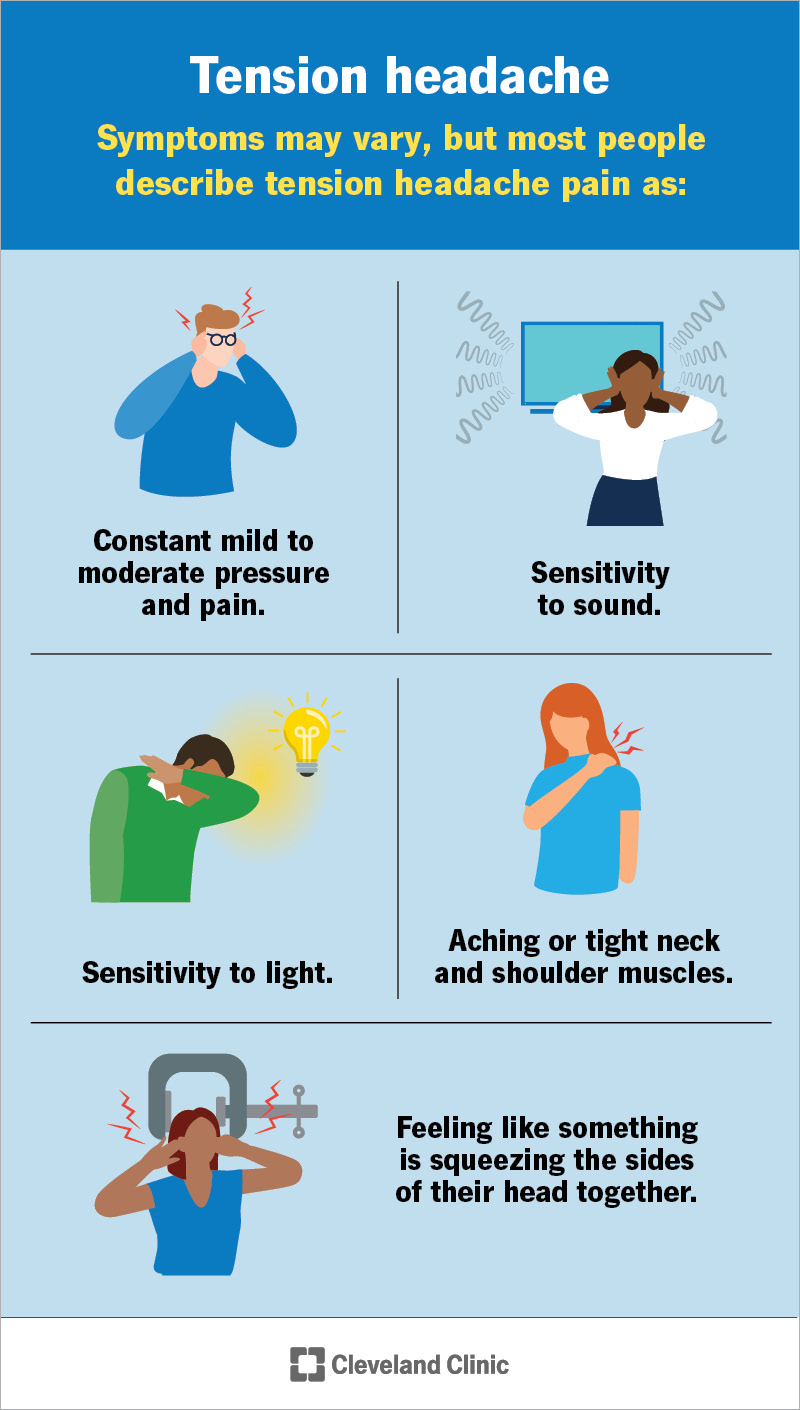
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/8257-tension-headaches)
Symptoms may vary, but most people describe tension headache pain as:
These symptoms may come on slowly. They may last about 30 minutes, but sometimes, they last as long as a week. Some people with chronic tension headaches may feel as if they’re always dealing with headache pain and pressure.
Researchers are still seeking a single cause for tension headaches. Some believe tension headaches start when muscles between your head and neck knot up, eventually tightening your scalp muscles. That muscular ripple effect may happen because you’re stressed or dealing with emotional conflict. Other tension headache causes include:
Advertisement
Chronic tension headaches that last for weeks and months may affect your quality of life. For example, a chronic tension headache may make it hard for you to focus on your work or family responsibilities because you’re always dealing with tension headache pressure.
Healthcare providers may ask about your medical history and symptoms, including questions like:
They may do computed tomography (CT) scans and brain magnetic resonance imaging (brain MRI) scans to check for underlying issues.
Treatments vary depending on the tension headache type. For example, if you have episodic headaches, your provider may recommend you start over-the-counter pain relievers like:
If you have chronic tension headaches, your provider may prescribe:
Side effects and complications vary depending on treatment, but rebound headaches are one common potential side effect of taking over-the-counter and/or prescription pain relievers for tension headaches.
Rebound headaches, or medication overuse headaches, are headaches that happen if you use headache medication too often. Healthcare providers recommend limiting pain relief use to 10 days in any given month.
If you’re like most people, you have episodic tension headaches that you can manage with pain relievers and by reducing stress. People with chronic tension headaches may need to take antidepressants or participate in therapy like biofeedback.
Managing stress may be the most effective way to prevent a tension headache. The most effective stress management tools are the ones that you can fit into your daily routine and make you feel good. Some examples include:
Advertisement
Over-the-counter pain relievers may help ease occasional tension headaches. Home remedies like placing a hot or cold compress on your head and neck may help.
Tension headaches aren’t life-threatening, but they can be a sign of a serious medical issue or that an existing issue is getting worse. Talk to a healthcare provider if you have a headache and you have:
You should go to the ER if you have a sudden severe headache that worsens quickly. You should also get immediate medical care if you have a headache and experience:
Advertisement
You may want to ask your provider:
Tension headaches start in your neck and shoulder muscles as your body deals with stress and other issues. Next, you feel a dull ache in your forehead, like someone’s got your head in their hands.
If that’s your situation, you may be having a tension headache. They may happen occasionally or they can be constant. Either way, talk to a healthcare provider if you have tension headache symptoms. They’ll ask questions to understand why you have these symptoms. If stress is the culprit, your provider also will recommend lifestyle changes and other things you can do to reduce stress and prevent tension headaches. In some cases, healthcare providers may recommend prescription medication or physical therapy.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Need care fast? Cleveland Clinic’s Express Care and Urgent Care locations treat everything from sprains to sinus infections — no appointment needed.
