Gestational diabetes is high blood sugar during pregnancy. Eating healthy, well-balanced foods and getting exercise can usually keep it well managed. But sometimes, insulin is necessary to help you manage blood sugar levels. If left untreated, it can cause health problems for both you and the fetus.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
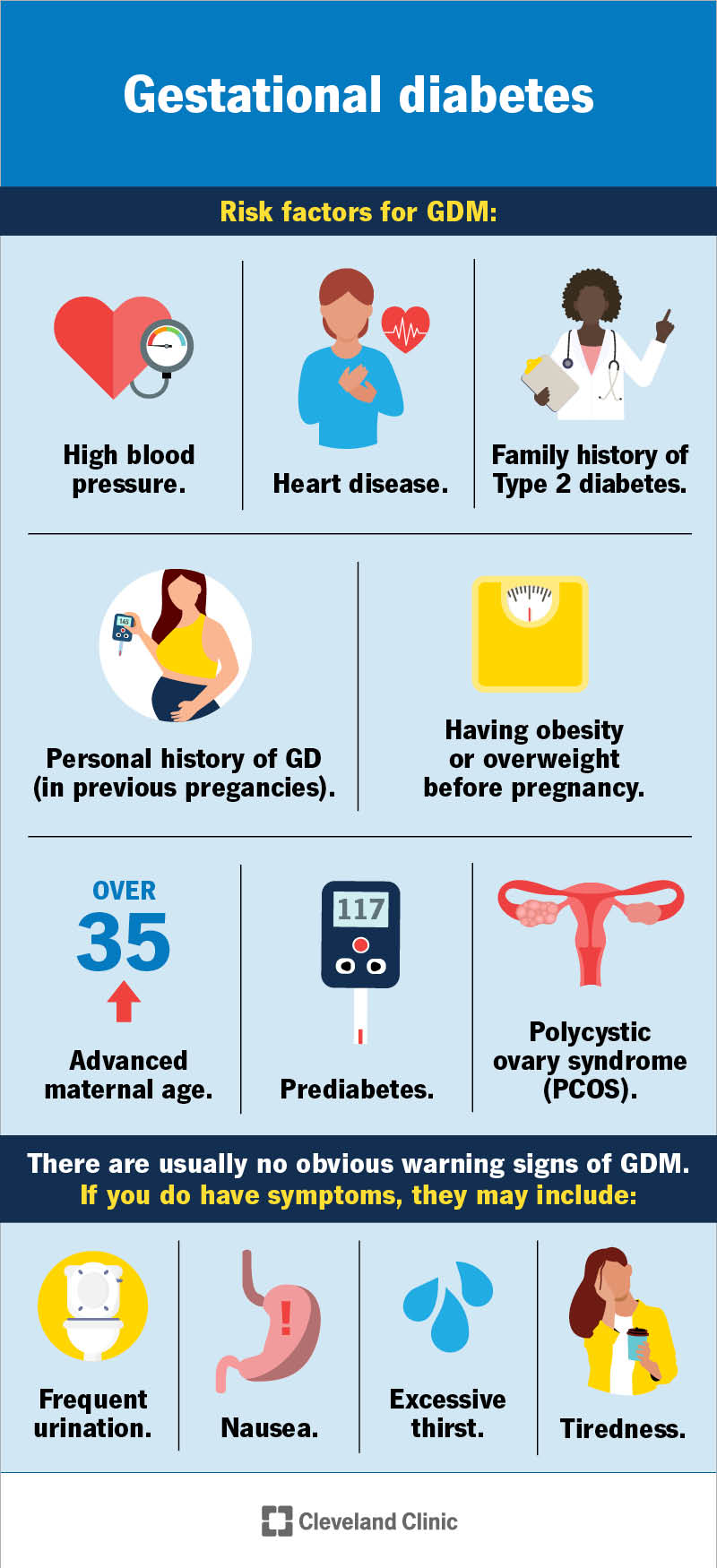
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9012-gestational-diabetes)
Gestational diabetes (GD or GDM) is a type of diabetes that develops exclusively in pregnancy when blood sugar levels get too high (hyperglycemia). It happens when the hormones from the placenta block your ability to use or make insulin. Insulin helps your body maintain the right amount of glucose in your blood. Too much glucose in your blood can lead to pregnancy complications. GD usually appears during the middle of pregnancy, between 24 and 28 weeks. Your pregnancy care provider will order a blood test to check for gestational diabetes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Developing GD doesn’t mean you already had diabetes before you got pregnant. The condition appears because of pregnancy. People with Type 1 and Type 2 diabetes before pregnancy have their own, separate challenges when they become pregnant.
Fortunately, gestational diabetes is well understood, and healthcare providers are usually able to help you manage the condition with small lifestyle and dietary changes. Most people don’t experience serious complications from gestational diabetes and deliver healthy babies.
If you have gestational diabetes, your pregnancy care provider will have you visit a nutritionist who specializes in gestational diabetes. At this appointment, you’ll talk about how certain foods typically increase blood sugar levels and how to make sure your meals and snacks contain the right types and amounts of food.
They’ll also talk to you about checking or testing your blood sugar at home, and what your levels should be after meals.
Finally, your obstetrician or nutritionist will discuss a gestational diabetes management plan. People with diabetes typically have more prenatal visits to check on fetal growth, monitor their weight gain and discuss how well they’re managing their blood sugar.
Advertisement
The rate of gestational diabetes in the United States is rising. According to the U.S. Centers for Disease Control and Prevention (CDC), about 8% to 10% of pregnant women will develop GD.
The rate of gestational diabetes worldwide, on average, is between 14% and 17%. Other factors can contribute to rates being higher, such as age, race/ethnicity, access to prenatal care and geography.
Gestational diabetes comes from hormonal changes and the way your body converts food into energy.
A hormone called insulin breaks down the glucose (sugar) from food and delivers it to your cells. Insulin keeps the level of glucose in your blood at a healthy level. But if insulin doesn’t work right or you don’t have enough of it, sugar builds up in your blood and leads to diabetes.
During pregnancy, hormones from the placenta can interfere with the way insulin works. It may not regulate your blood sugar levels like it’s supposed to, which can lead to gestational diabetes.
Anyone can get gestational diabetes during pregnancy. But certain factors can increase your risk. They include:
People over the age of 25 who are of South and East Asian, Hispanic, Native American or Pacific Island descent are also at a higher risk.
There are usually no obvious warning signs of gestational diabetes. Symptoms are mild and often go unnoticed until your pregnancy care provider tests you for gestational diabetes.
If you do have symptoms, they may include:
Being unable to keep your blood sugar levels in a healthy range can lead to complications for both you and the fetus.
Gestational diabetes increases your risk of:
People with gestational diabetes are slightly more likely to have Type 2 diabetes later in life.
If you have gestational diabetes, your baby’s more at risk for:
Your healthcare provider tests for gestational diabetes around weeks 24 to 28 of your pregnancy. Most healthcare experts believe this is the best time to get the most accurate results. But your provider may screen you for gestational diabetes a little earlier, especially if you have risk factors for the condition.
Advertisement
Your healthcare provider will test your blood sugar during pregnancy with a blood test. Often, the first test is a “screening,” which means it identifies people who are more likely to have gestational diabetes. If you don’t pass the screening, your provider will order a second blood test which is more comprehensive.
If you have gestational diabetes, you’ll need more frequent checkups during your pregnancy. Your pregnancy care provider will want to:
Advertisement
To keep track of your blood sugar at home, you’ll need a tool called a glucose meter. You’ll need the monitor itself, as well as needles (or lancets) and test strips. Taking your blood sugar involves pricking the tip of your finger with the lancet and then wiping the blood on a test strip. Then, you insert the test strip into the meter. After a few seconds, the device will display a number. This is your blood sugar level. Your nutritionist or diabetes educator will go over how to use the device. It may take a few days to get the hang of it, but your provider is always available to help you if you need it.
You’ll have to record your meals and blood sugar readings on paper, on an app or whatever way your provider wants you to. Then, your pregnancy care provider will review your readings at regular intervals (often weekly or biweekly). Sometimes, your provider will need to adjust your food (like decreasing the amount of carbs you eat) to keep your glucose levels well managed. The combination of tracking your blood sugar levels and eating diabetes-friendly food is usually enough to manage gestational diabetes.
Advertisement
Some people need medication such as insulin to manage gestational diabetes. This usually involves injecting insulin into your stomach, thigh or buttocks every day or multiple times a day. How frequently you need to inject insulin depends on many factors. Your healthcare provider will teach you how to inject insulin, when to take it and how much to take. If you need to use insulin to manage diabetes, it’s important to take it exactly as your provider prescribes.
You typically record your glucose levels right when you wake up (before eating anything) and then about one hour after each meal. For example, you may take your blood sugar upon waking up at 6:15 a.m. Then, if you eat breakfast at 7 a.m., you’d take your blood sugar level around 8 a.m. You record the numbers in whatever way you and your provider have agreed on.
The American College of Obstetricians and Gynecologists typically recommends the following ranges for blood glucose levels:
As always, everyone is unique, and these are only guidelines. Your pregnancy care provider will discuss what your blood sugar range should be.
You can help manage gestational diabetes by eating nutritious foods that don’t cause your blood sugar to rise to unsafe levels. Try to:
Some people with gestational diabetes find that small tweaks to what they usually eat are all that’s necessary to maintain normal blood sugar levels. Still, some find that they have to make more changes. It’s important to keep in mind that some people may be able to eat certain foods without a large impact on blood sugar, but you may not be able to. Remind yourself that everyone is different and unique.
Hydration is important during pregnancy, especially if you have gestational diabetes. But there are no studies that show drinking water alone will directly lower blood sugar.
Staying hydrated does help your body regulate your blood sugar, though. It helps dilute your blood, which makes it easier for your kidneys to get rid of excess sugar. Water can also help your body use insulin more effectively, which also contributes to regulating blood sugar.
Exercise helps your body use more glucose, which may lower your blood sugar. If you have gestational diabetes, talk to your healthcare provider about creating a safe exercise plan. Your exercise plan should be unique to your overall health and your fitness level before pregnancy.
You can’t reverse gestational diabetes once you have it. Your provider will test you for diabetes after your baby is born (usually between six and 12 weeks postpartum) to see if you still have it.
Gestational diabetes is a common condition and healthcare providers have a good idea of how best to manage and treat it. You’ll still have a healthy pregnancy and a healthy baby if you have gestational diabetes. Work with your healthcare provider to make sure you understand your treatment plan and how you can keep your blood sugar levels healthy.
Take time to understand the possible complications of not managing gestational diabetes. Your baby has a very good chance of being born healthy, but you must take steps to manage the condition. If your blood sugar levels are high several readings in a row, don’t wait to contact your provider. Let them know that your blood sugar levels are repeatedly high so they can adjust your foods or medication and help you. Gestational diabetes is manageable, but there’s a level of responsibility you must take to ensure your pregnancy is healthy.
Your blood sugar levels should come down after you give birth, when your hormone levels return to normal. Your pregnancy care provider will test you for gestational diabetes after your baby is born to confirm it’s gone (usually around six to 12 weeks postpartum).
But about 50% of people with gestational diabetes develop Type 2 diabetes later in life. Eating the right foods for your body and getting physical activity can help lower your risk. Your healthcare provider may recommend blood glucose tests every few years to watch for diabetes, especially if you have one or more risk factors.
Yes, having gestational diabetes may make your pregnancy high risk. Healthcare providers consider a pregnancy high risk when either you or the fetus (or both) has health conditions that increase your chances of having a pregnancy complication.
Yes. Most babies born are born healthy. There are some steps you can take to manage gestational diabetes during pregnancy to give your child the best start in life. Attending all your prenatal appointments and managing diabetes the best you can during pregnancy are the two best things you can do.
It’s not entirely preventable, but you can take steps to reduce your risk. Eating balanced and nutritious meals and getting regular exercise before and during your pregnancy are the best ways to reduce your risk of developing gestational diabetes.
Make diabetes management part of your daily routine. Create a schedule and stick to it. Try to:
Even if you’re being careful to manage your condition, there may be situations where you need to call your pregnancy care provider. Contact your provider if you have gestational diabetes and:
Yes, you can get gestational diabetes even if you ate healthy before or during pregnancy. There are several other factors that go into your risk of getting diabetes. Things like hormones and genetics play a major role and those factors are beyond your control.
But if you have gestational diabetes, eating healthy, nutritious foods is one of the best ways to manage the condition throughout your pregnancy.
Your pregnancy care provider just told you that you “failed” your glucose test and that you have gestational diabetes. A million questions may be crossing your mind. Did I cause this? Do I need to prick my finger the rest of my pregnancy? Will my baby be born healthy? These questions (and others) are normal to have. Fortunately, healthcare providers have a good understanding of gestational diabetes and how to help you manage it.
Most people can manage gestational diabetes with small changes to what they eat. A nutritionist or diabetes educator can help you with that. Still, some people need a medication called insulin to help keep their blood sugar in check. In most cases, well-managed gestational diabetes doesn’t have a major impact on your pregnancy. But you have to play an active role in managing the condition to make sure your pregnancy and your baby are healthy.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Gestational diabetes sometimes develops during pregnancy, but it’s treatable. Cleveland Clinic providers are here to help you manage your blood sugar.
