Pleural effusion is a collection of fluid around your lungs. Your provider has to get rid of this fluid with medicine or a procedure. Also, they need to diagnose and treat the condition that caused pleural effusion. Treatments range from medicine to surgery. Pleural effusion can happen more than once. Your outlook depends on what caused it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
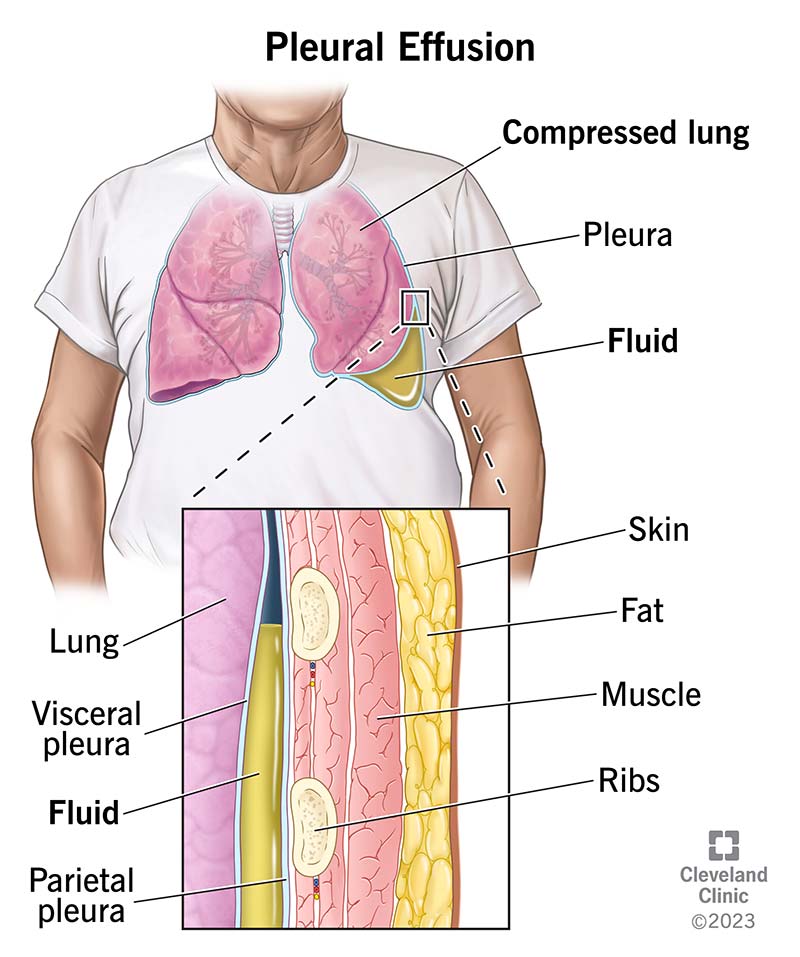
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/pleural-effusion)
Pleural effusion, which some people call “water on the lungs,” is the buildup of excess fluid between the layers of the pleura outside your lungs. The pleura are thin membranes that line your lungs and the inside of your chest cavity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Normally, everyone has a small amount of fluid in their pleura. This fluid acts as a natural lubricant and makes it easier for your lungs to move when you breathe. But with pleural effusion, you have too much fluid around your lungs. This means your body is producing too much of the fluid or not absorbing enough of the fluid it makes.
Healthcare providers split pleural effusion into two types, depending on the kind of fluid around your lungs.
Excess fluid may be:
Treatment varies by type and cause.
Pleural effusions are very common. Healthcare providers find pleural effusions in about 1.5 million people in the United States each year.
You may have unrelated symptoms due to the disease or condition that caused pleural effusion. Pleural effusion symptoms include:
Advertisement
Some people with pleural effusion have no symptoms. They find out they have pleural effusion when they have a chest X-ray for another reason.
There are many causes of pleural effusion, and some people have more than one.
Depending on the cause, the excess fluid may be either protein-poor (transudative) or protein-rich (exudative). These two categories help providers determine the cause of the pleural effusion. A pulmonary embolism (PE) can fall under either category.
The most common causes of transudative (watery fluid) pleural effusions include:
Common causes of exudative (protein-rich fluid) pleural effusions include:
Less common causes of pleural effusion include:
In some cases, the fluid itself may have malignant (cancerous) cells or may be a direct result of chemotherapy.
Risk factors for pleural effusion include:
Pleural effusion can lead to:
A provider will ask you about your medical history. They’ll ask what other illnesses you have and when your symptoms started. They’ll do a physical exam, which includes listening to your lungs when you breathe. Next, they’ll order tests.
Healthcare providers use these tests to diagnose and evaluate pleural effusion:
If less invasive tests don’t diagnose pleural effusion, you may need a thoracoscopy. Thoracoscopy is a minimally invasive technique, also known as video-assisted thoracic surgery, or VATS. A provider performs this while you’re under general anesthesia. Thoracoscopy allows them to see and evaluate your pleura. Often, they’ll treat your effusion during the thoracoscopy.
Advertisement
Treatment of pleural effusion focuses on getting the excess fluid out and keeping it from collecting again. Providers choose pleural effusion treatment based on the underlying condition and whether the effusion is making it hard for you to breathe.
Providers use diuretics and other heart failure medications to treat pleural effusion from congestive heart failure or other medical causes. Some people need antibiotics. For a malignant effusion, you may also need treatment with chemotherapy, radiation therapy or a medication infusion within your chest.
A provider can use therapeutic thoracentesis or a chest tube to drain a pleural effusion that’s causing respiratory symptoms.
Even with drainage, you may have pleural effusions that are hard to control or that come back due to a malignancy. In this case, a provider puts a sclerosing agent (a type of drug that purposely creates scarring) into your pleural cavity through a chest tube. This causes fibrosis (excessive fibrous tissue) of the pleura (pleural sclerosis). This is 50% successful in preventing pleural effusions from happening again.
You may need surgery if drainage or pleural sclerosis don’t work. Your surgeon will carefully evaluate you and discuss the possible risks and benefits of surgical pleural effusion treatments.
Advertisement
The two types of surgery include:
Complications of treatment may include:
You may need to take it easy for two days after a thoracentesis. If you have VATS, you may need to spend a few days in the hospital afterward. After a thoracotomy (open surgery), you’ll probably be in the hospital for a week.
You may have follow-up X-rays after you receive treatment. Your provider will want to make sure the treatment worked well. You’ll also need treatment for the medical condition that caused pleural effusion.
Advertisement
The seriousness of your condition depends on:
The outlook or prognosis varies depending on what caused your pleural effusion and what other conditions you have. For some people, pleural effusion treatment is successful. But pleural effusions can happen again. The outlook isn’t good when you have a pleural effusion from cancer. It’s also not good if you don’t get treatment for pleural effusion.
You may not be able to avoid the many causes of pleural effusion. But you can lower your risk of pleural effusions in these ways:
Some medical conditions that cause pleural effusion require long-term treatment. Be sure to talk with your provider about the best treatment for your chronic (long-term) condition. Then, stick to the treatment plan.
Go to all your follow-up appointments to manage your chronic condition. Get immediate help if you’re having trouble breathing.
You may want to ask your provider:
So you have pleural effusion and you may not have even had symptoms. Diagnosing the cause of it is key. Once your provider knows the cause, they can take steps to treat it. Answering their questions can help them rule out some potential causes. It can be scary when you have trouble breathing, so don’t be afraid to ask questions about anything you want to understand better.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
