Arthritis is extremely common, especially in people older than 50. It causes joint pain, stiffness and inflammation. Your provider will help you understand which type of arthritis you have, what’s causing it and which treatments you’ll need. You may need a joint replacement if you have severe arthritis that you can’t manage with other treatments.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/0_6mte9a0t/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn about the differences between osteoarthritis and rheumatoid arthritis.
Arthritis is a disease that causes damage in your joints. Joints are places in your body where two bones meet.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some joints naturally wear down as you age. Lots of people develop arthritis after that normal, lifelong wear and tear. Some types of arthritis happen after injuries that damage a joint. Certain health conditions also cause arthritis.
Arthritis can affect any joint, but is most common in people’s:
A healthcare provider will help you find ways to manage symptoms like pain and stiffness. Some people with severe arthritis eventually need surgery to replace their affected joints.
Visit a healthcare provider if you’re experiencing joint pain that’s severe enough to affect your daily routine or if it feels like you can’t move or use your joints as well as usual.
There are more than 100 different types of arthritis. Some of the most common types include:
Advertisement
Depending on which type of arthritis you have, it can break down the natural tissue in your joint (degeneration) or cause inflammation (swelling). Some types cause inflammation that leads to degeneration.
Arthritis is extremely common. Experts estimate that more than one-third of Americans have some degree of arthritis in their joints.
Osteoarthritis is the most common type. Studies have found that around half of all adults will develop osteoarthritis at some point.
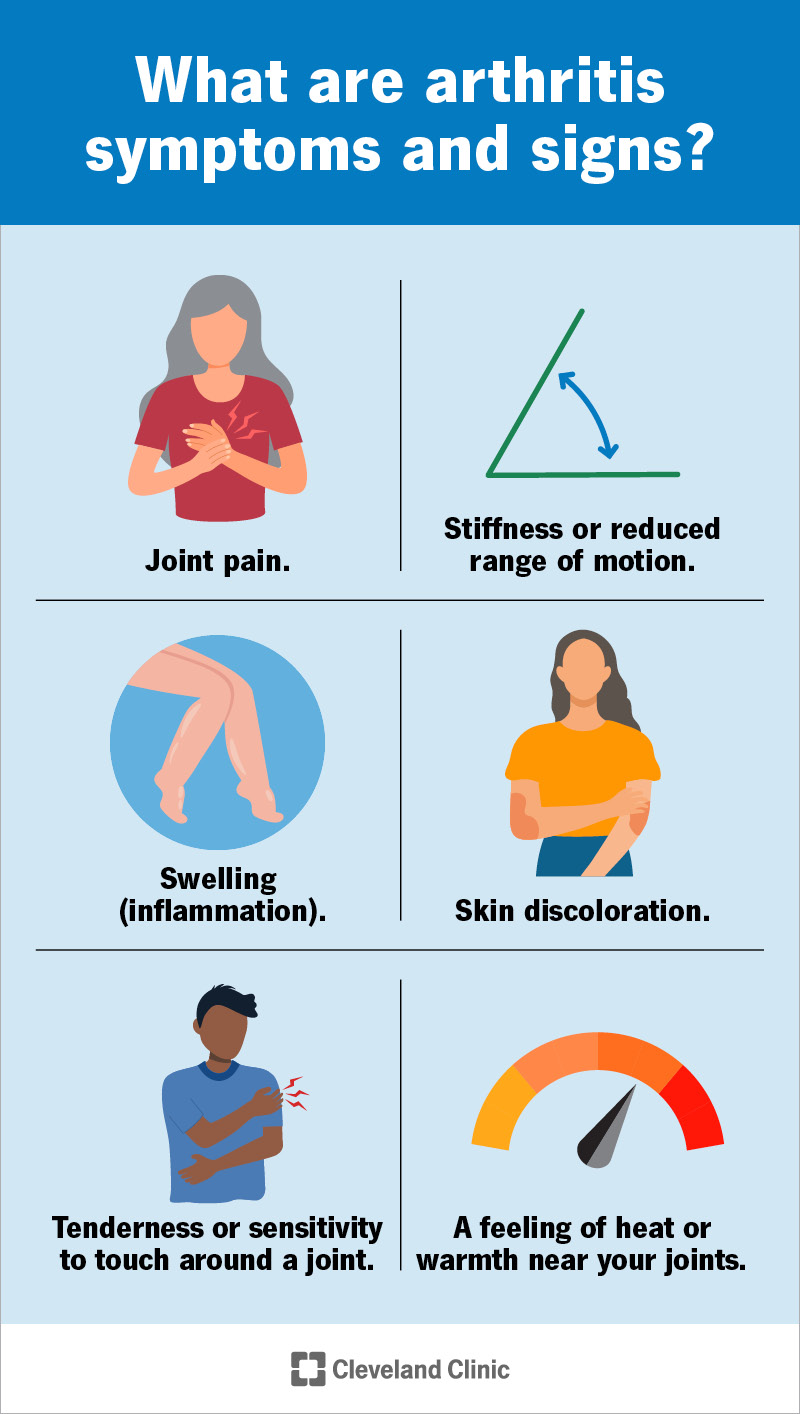
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/arthritis-infographic)
The most common arthritis symptoms and signs include:
Where you experience symptoms depends on which type of arthritis you have, and which of your joints it affects.
Some types of arthritis cause symptoms in waves that come and go called flares or flare-ups. Others make your joints feel painful or stiff all the time, or after being physically active.
What causes arthritis varies depending on which type you have:
Anyone can develop arthritis, but some factors may make you more likely to, including:
Some people have a higher arthritis risk, including:
Arthritis can develop at any age. When it starts depends on which type you have and what’s causing it.
In general, osteoarthritis affects adults older than 50. Rheumatoid arthritis usually develops in adults age 30 to 60.
Other types that have a more direct cause usually start closer to that specific trigger. For example, people with post-traumatic arthritis don’t develop it until after their joints are injured, and gout doesn’t develop until after you’ve had high uric acid levels for at least several months.
Advertisement
Talk to a healthcare provider about your unique arthritis risk, and when you should start watching for signs or changes in your joints.
A healthcare provider will diagnose arthritis with a physical exam. They’ll examine your affected joints and ask about your symptoms. Tell your provider when you first noticed symptoms like pain and stiffness, and if any activities or times of day make them worse.
Your provider will probably check your range of motion (how far you can move a joint). They may compare one joint’s range of motion to other, similar joints (your other knee, ankle or fingers, for example).
Your provider might use imaging tests to take pictures of your joints, including:
These tests can help your provider see damage inside your joints. They can also help your provider rule out other injuries or issues that might cause similar symptoms, like bone fractures (broken bones).
Your provider may use blood tests to check your uric acid levels if they think you have gout. Blood tests can also show signs of infections or autoimmune diseases.
There’s no cure for arthritis, but your healthcare provider will help you find treatments that manage your symptoms. Which treatments you’ll need depend on what’s causing the arthritis, which type you have and which joints it affects.
Advertisement
The most common arthritis treatments include:
You may need surgery if you have severe arthritis and other treatments don’t work. The two most common types of arthritis surgery are joint fusion and joint replacement.
Joint fusion is exactly what it sounds like: surgically joining bones together. It’s most common for bones in your spine (spinal fusion) or your ankle (ankle fusion).
If your joints are damaged or you’ve experienced bone loss, you might need an arthroplasty (joint replacement). Your surgeon will remove your damaged natural joint and replace it with a prosthesis (artificial joint). You might need a partial or total joint replacement.
Your provider or surgeon will tell you which type of surgery you’ll need and what to expect.
Advertisement
You should expect to manage arthritis symptoms for a long time (probably the rest of your life). Your provider will help you find treatments that reduce how much (and how often) arthritis impacts your daily routine.
Some people with arthritis experience more severe symptoms as they age. Ask your provider how often you should have follow-up visits to check for changes in your joints.
Some forms of arthritis happen naturally or because of health conditions you can’t change, so there’s not always a way to prevent it. However, you can lower your chances of developing arthritis by:
Visit your healthcare provider if you experience any of the following symptoms:
Questions you can ask your provider include:
Everyone’s body responds differently to different treatments, so there’s no one answer that works for everyone. Your provider will help you find a combination of treatments that relieves your arthritis pain. You might be able to take over-the-counter or prescription medicine as soon as you feel arthritis symptoms flaring up. Some people take arthritis medicine regularly to help prevent pain before it gets bad enough to affect their day-to-day activities.
Staying active is one of the best ways to relieve arthritis symptoms. Don’t force yourself to do anything that causes severe pain, but stretching and moving your body can reduce pain and stiffness and prevent them from getting worse.
You don’t need to become an ultramarathoner or Olympic weightlifter. Walking, swimming, riding a bike and stretching or doing yoga are all great ways to support your joints and strengthen muscles throughout your body.
Talk to your provider or physical therapist about exercises that are good for you. They’ll suggest options that help you safely stay active.
Some people find that their arthritis feels worse during certain types of weather. Humidity and cold are two common joint pain triggers.
There are a variety of reasons why this might happen. People tend to be less active in rainy seasons and winter. The cold and damp can also stiffen your joints and aggravate arthritis. Other theories suggest that barometric pressure (the pressure of the air around you), may have some effect on arthritis.
Talk to your healthcare provider if you feel like certain weather conditions or seasons make arthritis worse. They’ll suggest ways to prevent pain and stiffness throughout the year, or they may modify your arthritis treatments to fit any changes in your environment.
Arthritis is one of the most common health conditions people experience. But, just because lots of people have it, that doesn’t mean you should live in pain. Talk to a healthcare provider about ways to manage arthritis symptoms. They’ll help you find ways to spend more time doing the activities you love, and less time feeling stiff and uncomfortable.
Arthritis can be a pain in the neck (and knees, and hips, and back and any other joint in your body), but try to stay as active as possible. Ask your provider about physical or occupational therapy to help you stay strong, active and confident throughout your daily routine.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
